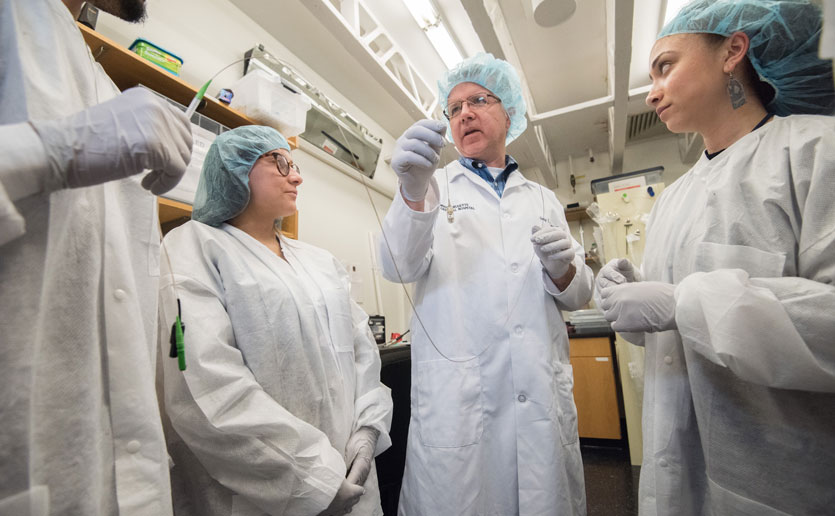
With a $2.79 million grant from The Leona M. and Harry B. Helmsley Charitable Trust, researcher Guillermo (Gary) J. Tearney, MD, PhD, can take the “gut probe” he invented to where it has never been.

The effectiveness of his swallowable capsule with its high-resolution microscope has already been demonstrated in scoping out problems in the upper part of the gastrointestinal (GI) tract. “But there are a lot of questions that need to be answered about how to use the same technology for the lower intestine,” says Dr. Tearney, who is the Remondi Family Endowed MGH Research Institute Chair. “We’re blazing new ground in trying to use our device there.”
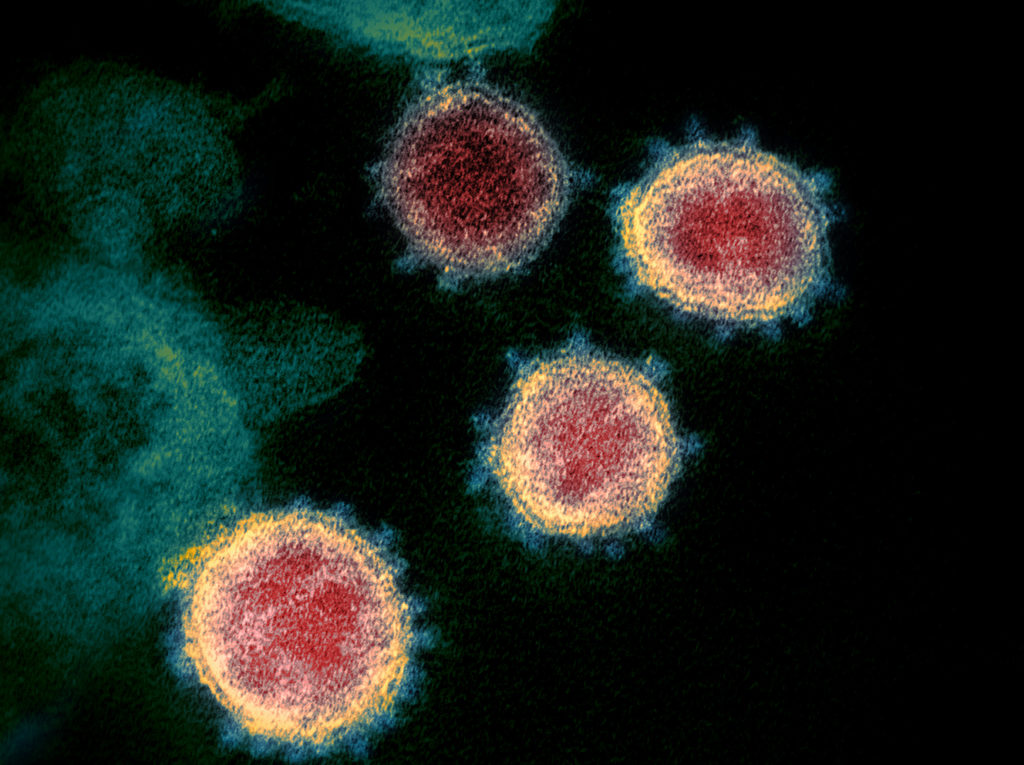
This effort, in partnership with the Helmsley Charitable Trust, aims in three years to expand the reach and capabilities of the device and test it in patients with Crohn’s disease. Because of continual inflammation, patients with Crohn’s disease experience debilitating flare-ups of diarrhea, abdominal cramps and pain throughout their lives.
Crohn’s is Helmsley Priority
The search for advancements in preventing, treating and eventually curing Crohn’s disease is one of the Helmsley Charitable Trust’s major program areas. Helmsley grants are typically bestowed by invitation only. They are given to research institutions and investigators whose work aligns with Helmsley’s program-based strategies “to improve lives by supporting exceptional efforts in the U.S. and around the world.”
Garabet Yeretssian, PhD, director of Helmsley’s Crohn’s Disease Program, reached out to Dr. Tearney after reading some of his scientific publications.
“This technology is a simpler, less invasive and faster way to go deeper than endoscopy has ever gone before.”
“I was very excited about the technology he developed,” says Dr. Yeretssian, who himself was a researcher focusing on Crohn’s disease and other GI diseases. “Our vision is to cure Crohn’s disease, but until we get there, we want to help every single patient live better with the challenges of this difficult and complex disease.”
Improvement in Diagnosis
A device like Dr. Tearney’s would be a big improvement for diagnosis, he explained. Diagnosis of Crohn’s disease is often delayed, especially in areas of the world like Asia where its incidence is rising.
“This technology is a simpler, less invasive and faster way to go deeper than endoscopy has ever gone before,” he says. “It will allow a lot of people — including infants — to get the best treatment at the right time and really improve their quality of life.”

Through the Crohn’s Disease Program, Dr. Yeretssian oversees nearly 100 Helmsley-funded initiatives focusing on Crohn’s disease. They encompass efforts to better understand the environmental triggers, genetics and gut microbiome origins of the disease. His team includes experts on Crohn’s disease, immunology, epidemiology and public health.
“Their experts are a tremendous resource as well as being partners in the development of the technology,” Dr. Tearney says.
Dr. Tearney has been able to develop his “crazy idea” for the gut probe thanks in part to philanthropic funding, as the Mike and Sue Hazard Family MGH Research Scholar from 2012-2017 and now as the Remondi Family Endowed MGH Research Institute Chair. This support has led to other funding to explore its applications — including from the National Institutes of Health and the Bill & Melinda Gates Foundation.
Current Uses
The gut probe is currently being used at Mass General to screen for Barrett’s esophagus, an early sign of esophageal cancer. It was piloted in adolescents with collaborators in Pakistan, where a disease associated with stunted growth and neurological development called environmental enteric dysfunction (EED) is widespread. A pilot using a smaller version to diagnose EED in infants starts there this spring.
“If it works, not only will it provide a good solution for Crohn’s, but it will probably also be relevant for many other diseases.”
There are problems to be solved to adapt the technology to reach the lower GI tract, Dr. Tearney says. The device needs to go a much longer distance along the twisting tube from the mouth through the stomach to the end of the intestines. After the capsule is swallowed, they need to be able to guide it safely in and safely out without damaging the gut.
How Low Can It Go?
It also must image cells not only on the surface, but through several layers of the intestinal wall to find the telltale signs of Crohn’s disease, inflammation and scarring. This capability does not currently exist. But when developed, the device could potentially also be used to screen for colon cancer and other lower GI tract conditions.
“This is our first attempt at going to the lower GI tract,” Dr. Tearney says. “If it works, not only will it provide a good solution for Crohn’s, but it will probably also be relevant for many other diseases.”
For more information about supporting research at Mass General, please contact us.
The Research Institute: Saving Lives Through Science
 The Massachusetts General Hospital Research Institute is the largest hospital-based research program in the United States, with a community of more than 8,500 people working across more than 30 institutes, centers and departments.
The Massachusetts General Hospital Research Institute is the largest hospital-based research program in the United States, with a community of more than 8,500 people working across more than 30 institutes, centers and departments.
Our researchers work side-by-side with physicians to pioneer the latest scientific advancements for curing disease and healing patients in Boston, across the United States and around the world.
To learn more about the Research Institute, please visit our website.