Slow or ineffective wound healing in individuals suffering from diabetes and the elderly causes enormous discomfort, increases the risk for infection and adds substantially to care costs.
A new therapy that can accelerate and improve wound healing showed early progress at Massachusetts General Hospital’s Vaccine and Immunotherapy Center (VIC), a research center dedicated to accelerating the development of broadly applicable vaccine and immunotherapies for infectious diseases, cancer and type 1 diabetes. VIC takes an entrepreneurial approach to research, offering project management support, as well as benchmarks for project advancement. Over the past nine years, VIC has developed seven products within its pipeline and partnered three products with pharmaceutical industry and US government agencies. VIC scientists rely on philanthropic support to move the most promising ideas forward in their early stages.
These results could have a profound impact on the quality of life of millions of individuals.
A Dramatic Improvement for Diabetics
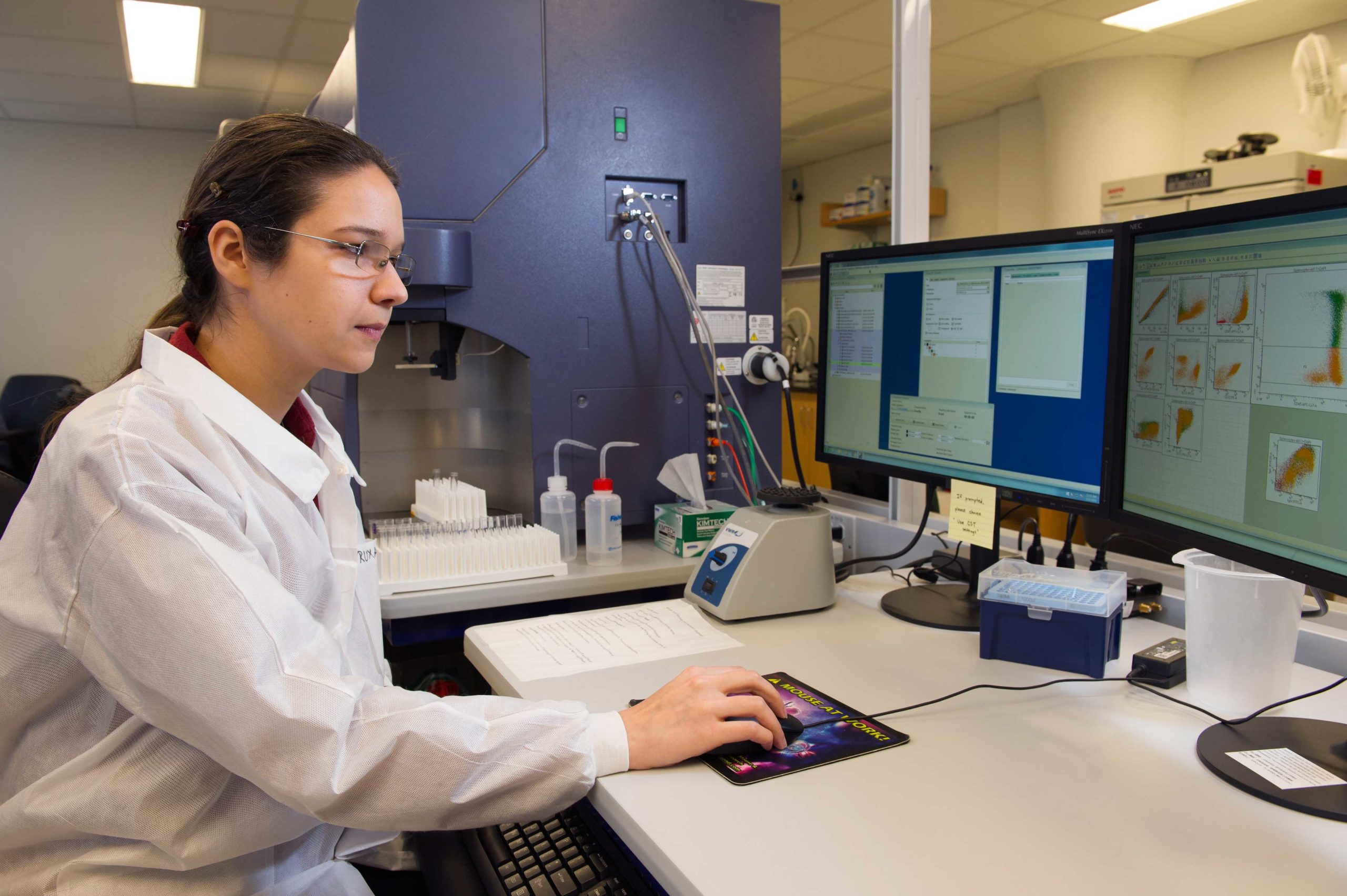
In a study led by Ruxandra Sîrbulescu, PhD, a senior scientist at VIC, and published in the journal Wound Repair and Regeneration in September, the researchers describe a dramatic improvement in wound healing using B cells isolated directly from spleen or blood. These results could have a profound impact on the quality of life of millions of individuals.
“We are using B lymphocytes, which are immune cells known primarily for their capacity to produce antibodies,” Dr. Sîrbulescu, a molecular biologist and neuroscientist says, “but we’re using them in a new way.”
“The wound closes remarkably quickly in our mouse models – days faster than in controls,” Dr. Sîrbulescu says. “With funding, we could bring this to a clinical trial in patients within the next 18 to 24 months.”

In a patient with a diabetic skin lesion, B cells would be isolated through a process called apheresis that can separate different types of cells in the blood. Then, the purified B cells would be applied topically to the wound.
A Simple Approach
Immunotherapy is making great advances in cancer treatment, with the FDA approving some therapies for specific types of cancer. The challenge of this therapy is that it requires extensive molecular manipulation of the blood cells after isolation before they are replaced in the patient’s body with a new set of instructions.
“The therapy we are developing for wound healing requires no cell manipulation. We are simply moving the right cell to the right environment, at the right time,” Dr. Sîrbulescu says. “In addition, this is a topical application, so it’s very simple to administer.”
Dr. Sîrbulescu says her research grew out of initial findings made by Mark Poznansky, MD, PhD, director of VIC, and has received enormous project support from VIC’s Senior Project Manager Ann Sluder, PhD, and the entire team at VIC.
Dr. Sîrbulescu has dedicated her career to regenerative neuroscience, studying ways to encourage the nervous system to repair itself.
Support Brings Therapy to Patients
“There are questions that need to be asked about FDA quality controls, regulations and patents that I, as a basic scientist, had not considered,” Dr. Sîrbulescu says. “The support I have received with these kinds of issues has saved me an enormous amount of time and moved this research forward quickly.”
Dr. Sîrbulescu has dedicated her career to regenerative neuroscience, studying ways to encourage the nervous system to repair itself.
“Our success with wound closure has already provided important information as we develop this therapy further, to tackle neuro-regeneration in the context of injuries to the central and peripheral nervous system,” Dr. Sîrbulescu says. “These findings are an enormous step forward.”
Private philanthropy plays an essential role in allowing Dr. Sîrbulescu’s research to advance. To learn how you can contribute to efforts to bring this therapy to patients who need it, please contact us.