In nature, diversity is typically a good thing. It’s why diverse ecosystems have a better chance of surviving a drought, and the reason farmers rotate their crops to prevent soil depletion.
The human female reproductive tract is unique among primates in that it is normally dominated by one species of bacteria — Lactobacillus.
When it comes to the microbial population in the human female reproductive tract (FRT), however, diversity is not desirable. It can actually cause a lot of problems.
The human female reproductive tract is unique among primates in that it is normally dominated by one species of bacteria — Lactobacillus. When that population is disrupted by the emergence of other types of bacteria, it causes a condition known as bacterial vaginosis (BV).
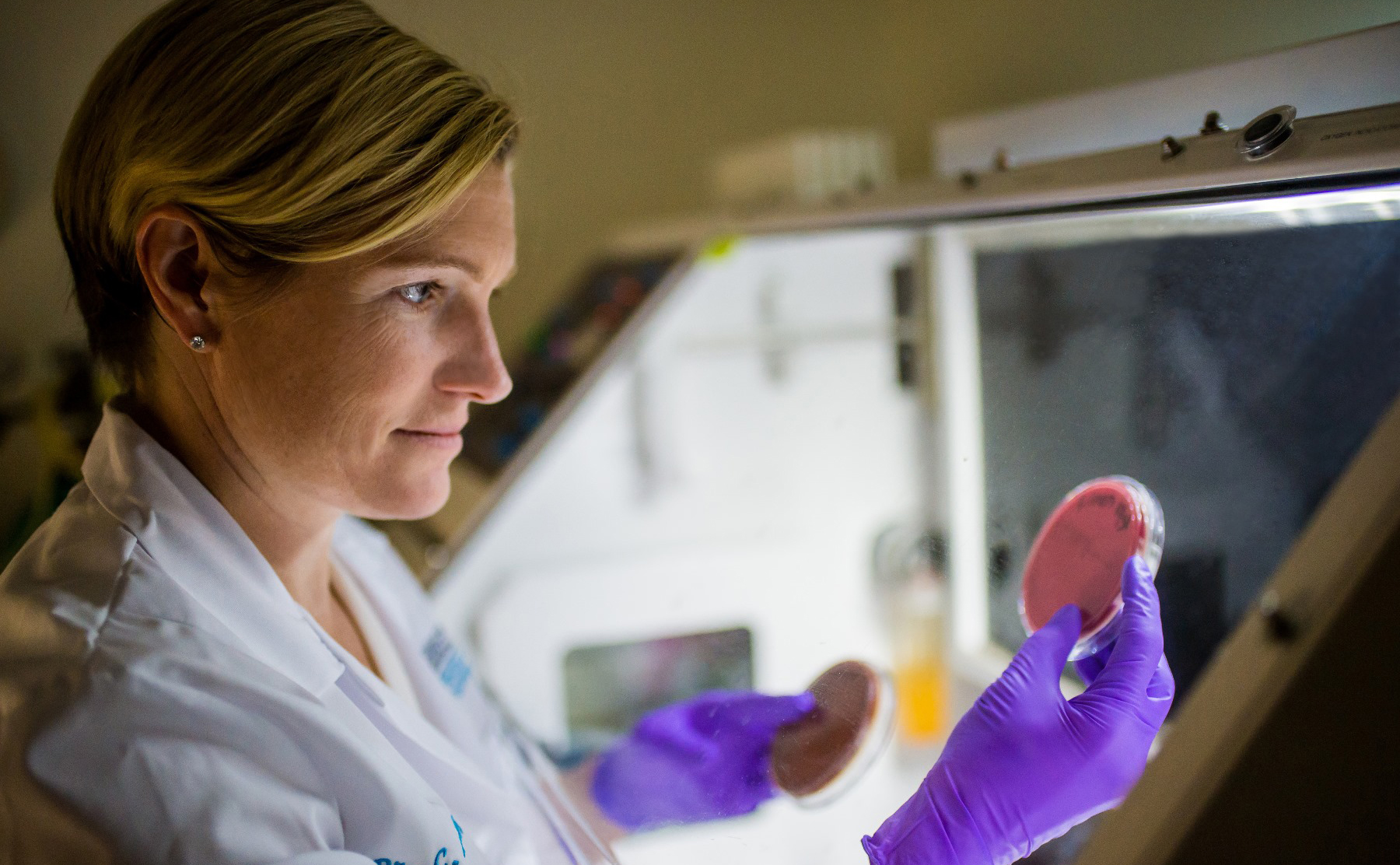
Caroline Mitchell, MD, MPH, researcher and clinical gynecologist at Massachusetts General Hospital, is hoping to learn more about how changes in the microbial population causes BV, and how BV affects the health outcomes of women of all ages.
It’s proven to be a challenging task from both a scientific and a social standpoint.
Health Implications of BV
Symptoms of BV can range from the unpleasant — including vaginal itching, odor or discharge — to the far more serious — including difficulty conceiving, a higher risk of premature delivery and low birth weight, and an increased risk of contracting sexually transmitted infections.
It’s still not known how BV develops, though risk factors include having new or multiple sex partners, douching and smoking. The condition often resolves itself but can also be treated with antibiotics.
While the symptoms of BV are unpleasant on their own, it’s the ensuing inflammatory response in the reproductive tract that leads to most serious health risks.
Recent research by Dr. Mitchell and her collaborators (including Douglas Kwon, MD, PhD, of the Ragon Institute) has shown that BV is associated with inflammation that likely is the cause of more serious complications.
“We haven’t had a fundamentally new treatment for BV in decades, and the current treatment doesn’t change the outcomes …”
If Dr. Mitchell and others can learn more about what causes BV and identify new treatment strategies to reduce inflammation, it could help to significantly reduce the risk of disease transmission and improve birth outcomes.
“We haven’t had a fundamentally new treatment for BV in decades, and the current treatment doesn’t change the outcomes, likely because the inflammatory response is already set off,” Dr. Mitchell says.
Searching for a Good Model System
While the unique Lactobacillus-dominant bacterial system of the FRT is interesting from scientific standpoint, it makes research challenging because there are no animal models that can be used to study how bacteria and host tissue interact.
Dr. Mitchell, whose lab is housed in the Vincent Center for Reproductive Biology at Mass General, first tried to overcome this challenge by studying human tissue samples obtained from hysterectomy patients.
“It seemed like a really good idea at the time, but turned out to be terrible,” she says, explaining that there was too much variation in immune response among the individual tissue samples for the researchers to draw any general conclusions.
Dr. Mitchell is now working with a research team at the Massachusetts Institute of Technology to create a unique synthetic tissue that replicates the layering of cells in the vagina by layering fibroblasts (structural tissue) and basal lamina (supportive tissue) underneath a layer of epithelial cells (similar to those lining the FRT).
This will essentially provide the team with a laboratory model made out of things they can control, she explains. “It’s like biological Legos.”
“Patients I see in the clinic will say, ‘Have you ever seen this before?’ I want to say, ‘I see this every day. You are not alone.'”
Communication Breakdown
In addition to the scientific challenges of her work, Dr. Mitchell also has to contend with the squeamishness that many people experience when discussing vaginal health.
“Talking about bacteria is totally above board for everyone,” she says. “Talking about vaginas is still uncomfortable for most people, even patients.”
By learning more about the scientific mechanisms of BV, Dr. Mitchell hopes to identify new treatment strategies and help BV patients feel more comfortable talking to their doctors.
“A more open discussion about symptoms of vaginal discharge and discomfort will help people realize how common these symptoms are, and how much we need better science, more treatments and a greater understanding of vaginal physiology so that women don’t have to suffer in silence anymore,” she says.
“One of the most striking things to me is that the patients I see in the clinic will say, ‘Have you ever seen this before?’ I want to say, ‘I see this every day. You are not alone.'”
To learn more about how you can support the work of Dr. Mitchell and other researchers at the Vincent Center for Reproductive Biology, please contact us.
This story first appeared on the Mass General Research Institute’s Web site.
The Research Institute: Saving Lives Through Science
 The Massachusetts General Hospital Research Institute is the largest hospital-based research program in the United States, with a community of more than 8,500 people working across more than 30 institutes, centers and departments.
The Massachusetts General Hospital Research Institute is the largest hospital-based research program in the United States, with a community of more than 8,500 people working across more than 30 institutes, centers and departments.
Our researchers work side-by-side with physicians to pioneer the latest scientific advancements for curing disease and healing patients in Boston, across the United States and around the world.
To learn more about the Research Institute, please visit our website.