Cancer cells routinely evade detection by the body’s immune cells, but a relatively new type of cancer drug, called a chimeric antigen receptor (CAR) T-cell, attempts to pierce that defense. For some cancers — most notably, some lymphomas and leukemias — CAR T-cell drugs are making a significant difference for patients.
“There have been some pretty amazing responses — including long-term responses — in patients who had many prior therapies with chemotherapy and multiple standard cancer drugs,” says Marcela Maus, MD, PhD, director of the Cellular Immunotherapy Program at the Mass General Cancer Center. While CAR T-cell drugs have captured the attention of the public and further solidified immunotherapy as a viable treatment option, the impact is still largely limited to cancers of the blood. But thanks to the efforts of Dr. Maus and the members of her lab, CAR T-cell drugs may soon be available to treat a wide range of cancers.
Redirecting the Attack
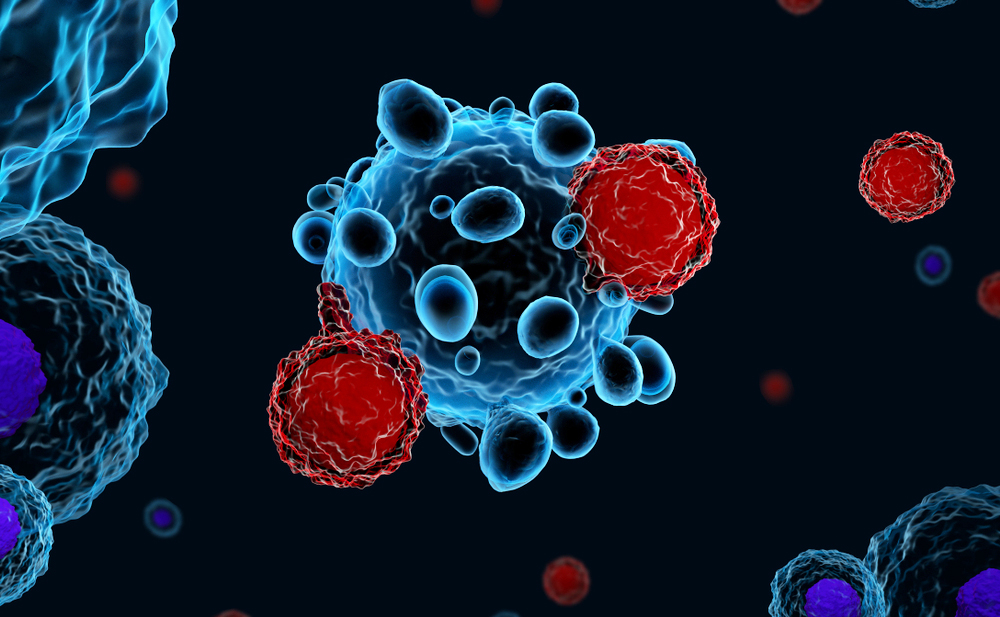
Broadly speaking, a CAR is any synthetic molecule that commands the T-cells of the immune system to identify and stick onto a specific target, or antigen, such as a tumor cell. CAR T-cell treatment involves reengineering a patient’s own T-cells in the lab, so they are equipped to recognize and target tumor cells.

First, scientists search for the molecules that T-cells rely on to recognize a foreign antigen and attack it — in this case, the patient’s cancer. Then, a gene that codes for making that CAR is inserted into the T-cells in the laboratory.
“That way, the T-cells keep their own biology but now have this extra CAR gene to produce a receptor that allows them to recognize and kill tumors,” says Dr. Maus. “Then we give them back to the patient, and they go to work.”
Finding New Targets
Today’s FDA-approved CAR T-cell therapies home in on targets present on certain types of lymphomas, leukemias and myelomas. “But CARs can be designed to recognize any multitude of antigens on tumor cells,” says Dr. Maus.
As an example, with support from generous donors, the Maus lab has developed a new CAR T-cell therapy, now in a Phase 1 clinical trial at Mass General that targets T-cell lymphoma, which presently does not respond to CAR T-cell therapy. To date, four patients have been treated, including at least one who had a complete response.
“This is one of the advantages of working at Mass General,” says Dr. Maus. “We designed something in the lab that we took all the way to patients without it ever leaving the hospital.”
Zeroing in on Solid Tumors
One cancer type where CAR T-cell treatment has so far proven ineffective is solid tumors — which are characteristic of brain, pancreatic and ovarian cancers. Toward that goal, Dr. Maus’ team is designing a new kind of CAR T-cell therapy that secretes another molecule. Because T-cells actively cross the blood-brain barrier, Dr. Maus is harnessing that ability to use CAR T-cells as carriers to deliver other therapies into the tumor environment.
“With that technique, we are targeting multiple antigens that bring bystander T-cells into the brain tumor microenvironment,” explains Dr. Maus. It also attracts other kinds of T-cells that normally keep the immune system quiet and converts them into cancer-killing cells. The approach will be part of a clinical trial for glioblastoma, an aggressive brain cancer, in late 2021.

Philanthropy Essential to the Mission
The kind of bench-to-bedside work that Dr. Maus and her group focus on is generally not funded by foundations, government institutions or biotech partners. “That’s where philanthropy is essential,” added Dr. Maus. In the case of her CAR T-cell research, donations from the Loring family enabled the first clinical trial of a new CAR T-cell therapy for patients with lymphoma. “Because of that support, we’ve set up a lot of infrastructure now to build out the program for lymphoma, myeloma and solid cancers,” Dr. Maus says.
“The first one is the toughest and if we are successful, we will be able to apply this bench-to-bedside strategy to multiple diseases. Then, once we show we can make an impact in patients, we hope to attract industry to scale it up further so it can be available not just at Mass General but also to the national and global communities.”
To learn more about how you can support cell therapy research at Mass General, contact us.

This story is just one example of the groundbreaking efforts taking place at Mass General, home to the largest hospital-based research enterprise in the U.S. — the Mass General Research Institute. The Research Institute encompasses and provides support to thousands of scientists, hundreds of laboratories, and helps to guide, connect and promote this unrivaled community of investigators as they advance the future of medicine, from the bench to the bedside, to the community and world.