Felipe Pincinato will never meet the person who saved his life.
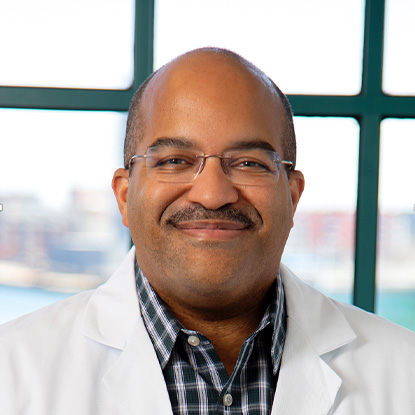
In 2023, when Felipe was 18 years old, and ready to leave his hometown of Jundiai, Brazil, to start college, he was diagnosed with an incurable form of lymphoma. Today, he is in full remission, thanks to the generosity of an anonymous Massachusetts General Hospital patient and the expertise of hematopathologist and investigator, Abner Louissaint, Jr, MD, PhD, and his research team.
It started with a lump in his neck, like a pea under his skin. Felipe didn’t think much of it at first, and neither did the doctors at his regional hospital who prescribed anti-inflammatory medications and sent him on his way. But two weeks later, the pea had grown to the size of a marble, and another lump had started to form.
A battery of tests delivered a diagnosis that left his care team puzzled: ALK+ large B-cell lymphoma, a fast-growing blood cancer with fewer than 200 published cases. This was something the care team had never seen, let alone treated. They started Felipe on chemotherapy, hoping they could put the cancer in remission. But the cancer continued to spread unabated, and Felipe and his doctors started a desperate search for an alternative approach.
Patient-Powered Pathology
Years before Felipe’s diagnosis, and half a world away, an anonymous Mass General patient battling the same rare lymphoma made a fateful decision. Faced with a terminal diagnosis, this patient donated a sample of his tumor for research, in the hope that it might one day help others. That tissue was used by Dr. Louissaint’s team to create the first patient-derived model of ALK-positive large B-cell lymphoma.
“Clinical trials are the reason we’ve made the progress we have in cancer therapeutics,” Dr. Louissaint says. “The problem we run into is that that some of the most aggressive types of lymphoma are so uncommon that clinical trials are not possible. You could never recruit enough patients.”
Dr. Louissaint and his team specialize in the study of aggressive, and often incurable, B- and T-cell lymphomas. Using tumor fragments taken from patient samples, they create living models of these rare lymphomas, called patient-derived xenografts (PDXs). These unique PDXs allow them to study the biology of the individual cancers, test new and established therapies and identify biomarkers that can be used to predict response to therapies in future patients.
“Ultimately, we hope this work will lead to curative therapies for these aggressive lymphomas,” Dr. Louissaint says.
A Positive Result
As it turned out, ALK+ large B-cell lymphoma was the perfect candidate for this approach. ALK+ large B-cell lymphomas are driven by abnormal ALK proteins. While the rarity and aggressive nature of ALK+ large B-cell lymphoma meant it had gone largely unstudied, these ALK proteins, which also play a role in some lung cancers, have been a target for drug developers since their discovery in 2007. By the time of Dr. Louissaint’s study, three iterations, or “generations,” of ALK-targeting inhibitor drugs were available.
“Although first generation ALK inhibitors had been tested in these lymphomas and failed, we decided to test them all in our PDXs,” he says.
As predicted, the first generation ALK inhibitor failed to produce an effect in the model, but the second and third generations eliminated the PDX tumors completely. After confirming the results, Dr. Louissaint’s Mass General colleague and collaborating oncologist, Jacob Soumerai, MD, led a study with the Mayo Clinic, Memorial Sloan Kettering and other peer institutions, investigating this experimental approach with other ALK+ large B-cell lymphoma patients. The ALK inhibitors were tested in four patients, and in each case, they induced a complete regression of the tumors. And while the lymphoma would eventually return, the response provided patients with the necessary time to undergo a stem cell transplant, which eliminated the cancer entirely. To date, these patients remain in clinical remission.
“The reward for all of our hard work is seeing how the science can change people’s lives.”
Dr. Louissaint, Dr. Soumerai and their colleagues published their findings in the fall of 2022, and the National Comprehensive Cancer Network — the nation’s leading consortium of cancer centers — quickly adopted the protocol as part of the recommended guidelines for the treatment of ALK+ large B-cell lymphoma.
Living His Life
It was late February 2024, and Felipe’s father, Emerson, had started to panic. Felipe’s care team at Albert Einstein Israelite Hospital in Sau Paulo had discovered Dr. Louissaint’s study in December, and it had been several weeks since Felipe had started the “next generation” regimen — but it didn’t seem to be having an effect. So, one Saturday night, desperate, Emerson emailed Dr. Louissaint.
The response came almost immediately. “Can you talk now?”
That night, Dr. Louissaint talked Emerson through the protocol; he answered his questions and emphasized the limited time window for a transplant should Felipe’s disease go into remission.
Shortly after that phone call, Felipe started responding to the regimen, and by May, a PET scan showed he was cancer-free. By the end of the year, Felipe had undergone a stem cell transplant and was in full remission. Throughout the treatment and after, Felipe and Emerson stayed in close touch with Dr. Louissaint.
“Abner’s support meant so much to me,” Emerson says. “I’m so grateful.”
For Felipe, his experience with the next generation ALK inhibitor treatment was a far cry from his experience with chemotherapy. There was no exhaustion, no discomfort, no nausea. He carried on with life throughout, hanging out with his friends, and traveling an hour each way to his college to attend classes.
“With this, I could keep living my life,” says Felipe, who is majoring in mathematics and hopes to become a university professor.
A Rewarding Model
The Louissaint Lab is currently creating patient-derived models of other aggressive lymphomas, including plasmablastic lymphoma, diffuse large B-cell lymphoma and aggressive T-cell lymphomas, to make additional discoveries and identify new effective therapies. This work is made possible by individuals who consented to participate in research, and by the generous financial support of donors such as Aziz and Nur Hamzaogullari, longtime supporters of Dr. Louissaint’s research. In addition, Dr. Louissaint recently received a Krantz Family Center for Cancer Research Spark Award for his work using patient-derived models to identify novel therapeutic targets for plasmablastic lymphoma.
As a pathologist, rather than a clinician, Dr. Louissaint seldom interacts with patients, but he says getting the opportunity to meet with patients like Felipe is deeply gratifying.
“My passion is using patient-derived models of aggressive lymphomas to discover new and effective therapeutic options for aggressive lymphomas,” he says. “And the reward for all of our hard work is seeing how the science can change people’s lives.”
To learn more about how you can get involved in this and other cancer research efforts at Mass General Brigham, contact us.