In the fall of 2017, George “Doc” Lopez knew he was losing his battle with Parkinson’s disease. Parkinson’s disease (PD) is an incurable brain disease marked by a gradual loss of the cells that produce dopamine — a neurotransmitter linked to motor control and coordination. Since Doc’s diagnosis a decade earlier, the retired founder and CEO of ICU Medical, had relied on medication to help him ward off symptoms of the disease — which include tremors, stiffness and difficulty with speech and walking. But the medicine had finally run its course, and Doc was running out of time.
“Parkinson’s is like a cage around your body that gets smaller and smaller.”
“Parkinson’s is like a cage around your body that gets smaller and smaller,” says Doc, now 72, who began his career as a physician. “Patients would sometimes explain to me what dying felt like —and I finally knew what they meant.”
But then Doc underwent an experimental procedure to replace the cells he’d lost to PD. Using cells from Doc’s skin, a team of physicians and scientists from Mass General’s Department of Neurosurgery and McLean Hospital was able to engineer and implant new dopamine cells.
Two years later, Doc’s symptoms have improved, and he has regained some of his former mobility. While doctors hesitate to call it a cure, the revolutionary technique, recently revealed in the New England Journal of Medicine, shows the potential of personalized cell therapy to treat neurological diseases. And with the help of a transformational gift of $18.5 million from Doc, Mass General’s Department of Neurosurgery hopes to one day bring cell therapy to the millions of people suffering from PD and other neurological diseases.
A New Path to Treat Parkinson’s
Since it was first described in 1817, scientists have struggled to find a way to treat PD. But the advent of stem cell technology, roughly a decade ago, proved to be a source of hope for some patients.
In stem cell technology, scientists introduce certain proteins into mature cells. This process turns back the developmental clock, transforming these cells into stem cells. These new stem cells can then be coaxed to become genetic replicas of any of the 220 types of cells in the human body — including neurons, the building blocks of the brain.

In 2013, Doc approached Kwang-Soo Kim, PhD, a neurobiologist at McLean Hospital, who was exploring the potential of using personalized stem cells to treat PD. Impressed by Dr. Kim and his research, Doc offered to help fund the project. For four years, Dr. Kim refined techniques for creating dopamine cells and safely transplanting them into animal models to test their function and safety.
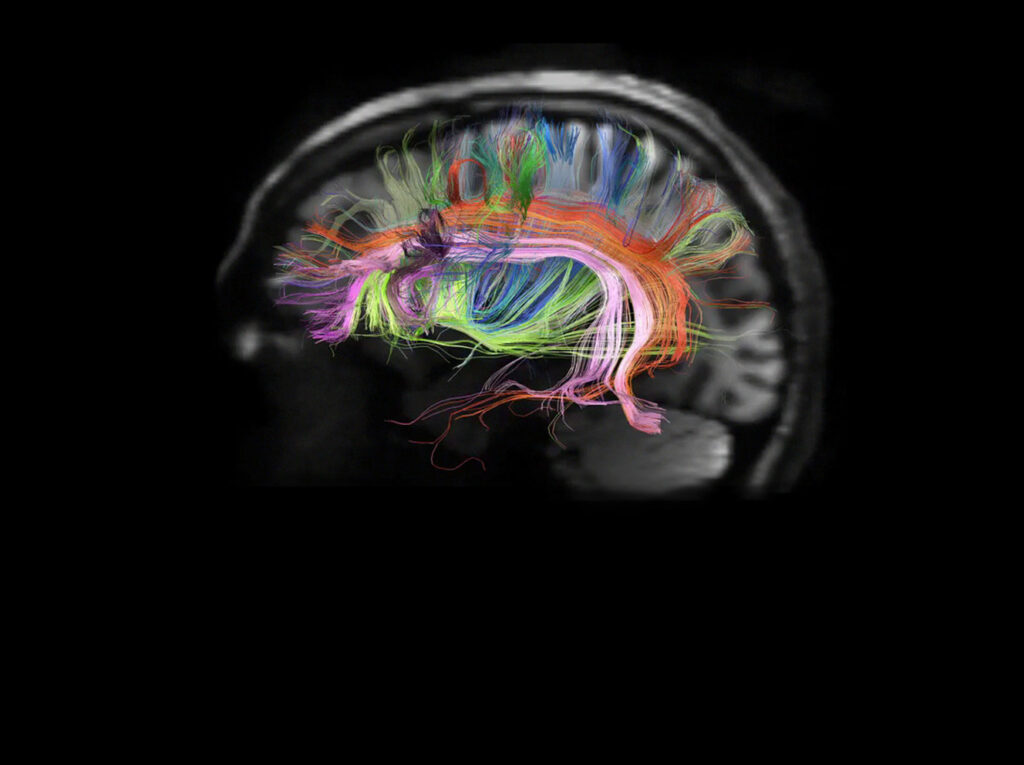
While stem cells have been used to treat some forms of cancer, PD has long been considered a disease of interest for stem cell researchers. “In the case of PD, the cell loss is confined to a particular region of the brain — the substantia nigra — which gave us a defined target,” says Bob Carter, MD, PhD, chief of Neurosurgery at Mass General, who joined the project in 2015.
With the new therapy ready to be tested, the team needed a patient. Doc volunteered. After thorough reviews by the FDA and the Partners Institutional Review Board, Doc and the team were cleared to proceed with the experimental procedure.
To reach the target area in Doc’s brain, the team used a new minimally invasive computer-guided syringe developed by Mass General neurosurgeon Jeffrey Schweitzer, MD, PhD, which delivered the cells at a specified rate to help ensure their even distribution and survival. While the planning took months, the actual procedures, involving both Dr. Carter and Dr. Schweitzer, were conducted in two three-hour sessions.
“There is always some risk in being the first patient treated with a new technique, especially one that involves brain surgery,” says Dr. Carter. “There’s a certain unknown in placing new cells into the brain. Will they cause an intense inflammatory reaction? Could these cells have some unintended effect?” Imaging tests conducted periodically since the procedure indicate that the cells are still alive and functioning. Mass General research neurologist, Todd Herrington, MD, PhD, has monitored Doc’s symptoms closely and has been pleased with his progress since the cell transplants.
Hope for the Future
“I want to treat a million patients with the technology we developed and leave this world knowing that it’s a better place.”
Dr. Carter hopes that Doc will be the first of many to benefit from the procedure. “It took a tremendous amount of effort to get us to this point,” he says. “But now, with Doc’s help, we’re going to evaluate it for a larger number of patients. Our vision is that we will establish Mass General as a global hub for cell therapy for patients with neurological diseases like PD — and this moves us forward.”
Doc is more direct. “I want to treat a million patients with the technology we developed and leave this world knowing that it’s a better place.”
He also believes that others can learn from his particular approach to philanthropy. “I’ve always believed that philanthropy is at its most powerful when you’re able to concentrate your funding in one area,” he says. “Spend your money on the best people, give them the best equipment and the resources they need. That’s all it takes.”
To learn more about how you can support personalized cell therapy, please contact Sarah Gaylord, Major Gifts, Department of Neurosurgery.