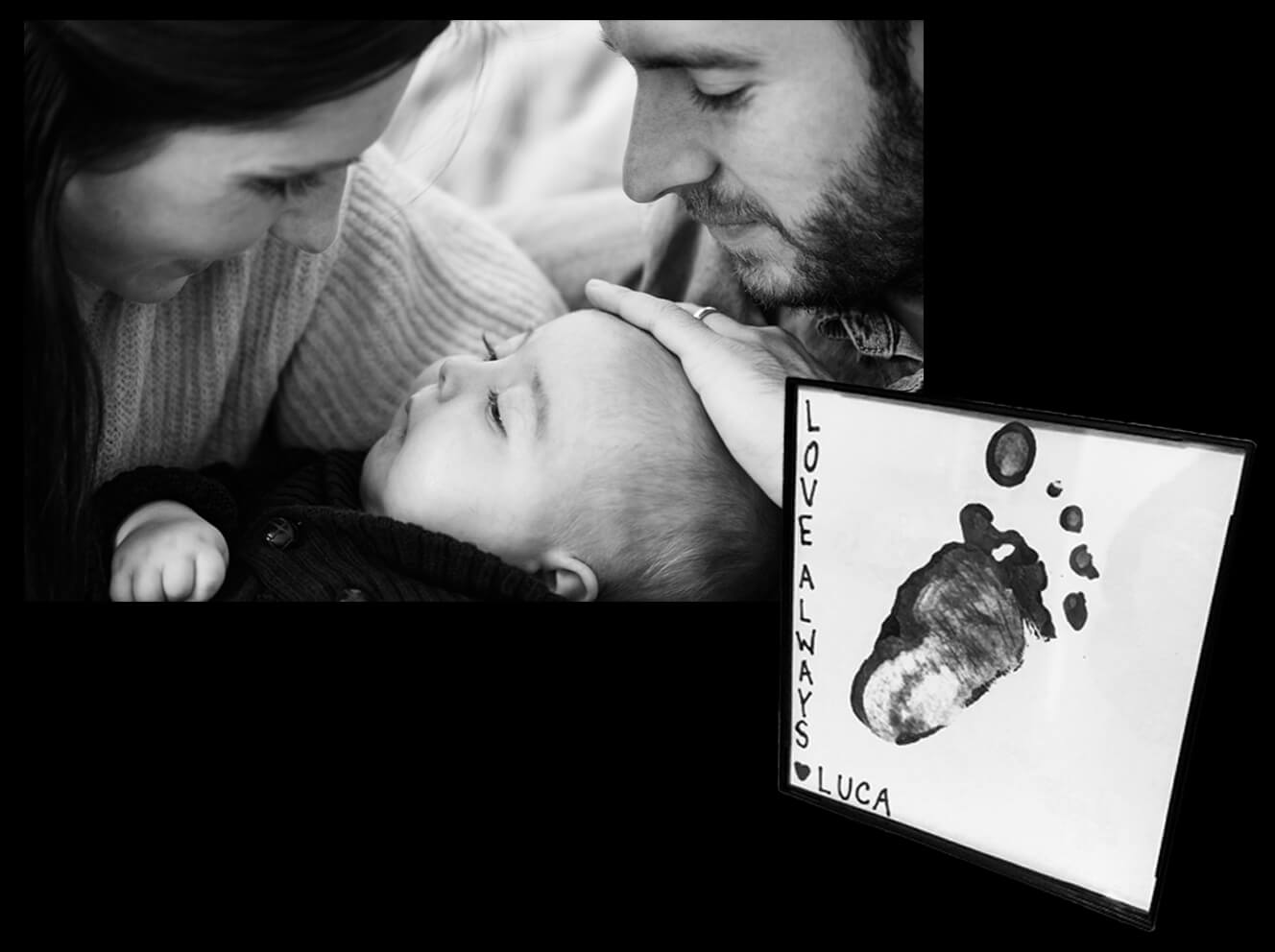
In a sense, Luca Lagarce has become immortal. This is not just because so many people remember him with love and affection, but because researchers at Mass General for Children (MGfC), using a biopsy from his skin, have grown pluripotent stem cells, which do not age, and continue to live indefinitely. Luca’s cells are helping to build the research infrastructure to someday uncover more information about CACNA1E — a mysterious gene that took Luca’s life when he was only nine and a half months old.
Luca came into the world in emergency circumstances. His mother, Brittany, had a rare condition called acute fatty liver, forcing her to have a cesarean section to save both of their lives. After one week in the neonatal intensive care unit (NICU) and four weeks in a special care nursery — to resolve some breathing issues that were presumed related to his emergency delivery — mom, dad and baby headed home. They were nervous. They were excited. But mostly they were hopeful the worst was behind them. Little did they, or anyone, suspect that this perfect baby boy with the longest eyelashes and the brightest of eyes was fighting a rare genetic disorder.

The Early Days
Like most first-time parents, Brittany and her husband Dave dove headfirst into parenting, unsure of what to expect. Parents of healthy newborns are often overwhelmed in the first weeks home, but when a child is experiencing undiagnosed health problems, that feeling is almost unbearable.
As time went on, Luca was becoming increasingly irritable, and it proved almost impossible to figure out why. He had reflux, so gastrointestinal physicians joined his care team. He continued to need the care of the neurology team for seizures he had been having since he was three weeks old. He was having difficulty swallowing. He developed a condition called laryngomalacia — a defect of the voice box — for which he needed surgery. He wasn’t growing at a normal pace. He wasn’t sleeping much. Something was not right.
After five months of struggling with these difficulties, the new family ended up back at MGfC, with Ann Murray, MD, MPH, Luca’s pediatrician, as primary advocate, and surrounded by multiple teams of specialists who were determined to unlock the mystery of Luca’s illness.
“At one point, there were more than 20 people in the room discussing different aspects of Luca’s care. It was overwhelming — but we truly appreciated the collaboration that was evident across all of Luca’s care teams,” recalls Dave.

The Search for a Diagnosis
It was during one of these multidisciplinary discussions that David Sweetser, MD, PhD, chair of the Division of Medical Genetics and Metabolism, got involved.
“We are commonly called on when issues are complex, and the diagnosis isn’t completely clear,” explains Dr. Sweetser. “We ran a series of metabolic tests to see how his body processed food and got rid of toxic byproducts. None of these tests pointed us in the right direction.”
Hypothesizing that Luca’s seizures and abnormal brain wave activity might hold the key, the neurology team started some therapies.
“This significantly reduced his irritability,” says Dr. Sweetser. “Everyone figured we were now on the right track. So, we sent off our first genetic test: a targeted panel looking at 151 genes that are known to cause seizures. They were negative. So, we moved on.
“The next step was to broaden our search. We sent off a larger panel that sequenced 23,000 genes, all the protein coding genes in the body. This time we got our answer. But sadly, it wasn’t the news we wanted to hear.
“Luca had a mutation in a calcium channel gene. This gene, known as CACNA1E, can cause seizures, and was only identified for the first time in 2018. The literature indicates that there are only 20 to 30 cases of this disease known worldwide. The prognosis is not promising. Most of these children pass away young.”

Certainty in a Sea of Unwelcome Choices
Dr. Sweetser had the unenviable task of sharing the news with Brittany and Dave.
“When Dr. Sweetser told me about the genetic mutation, I immediately felt guilty, like I had caused my child’s suffering,” says Brittany. “But Dr. Sweetser was adamant that was not the case. It was a spontaneous mutation, he told us, that neither Dave nor I carried.”
Brittany and Dave were now in a quandary. They had tried all available treatment options. What should they do now? Was there something they hadn’t thought of yet? Should they stay in the hospital or should they keep Luca home? Were those the only options they had? Were those even real options?
What they didn’t question however, was their decision to donate some of Luca’s skin cells to science. Dr. Sweetser told them about research taking place that involves turning skins cells like Luca’s into pluripotent stem cells, which means they can reprogram them to grow into different types of cells and tissues, including brain tissue. They can then study those cells and “quite literally start screening thousands of agents trying to look for medications that work better for babies born with the CACNA1E gene mutation,” says Dr. Sweetser. Brittany and Dave also set up Luca’s Legacy Fund to raise money to support Dr. Sweetser’s research in genetics.
Brittany and Dave found comfort in contributing to Dr. Sweetser’s important work, but not knowing how much time they had left with their little Luca brought great sadness. And so began a new chapter in the family’s journey …
To make a gift in support of Dr. Sweetser’s research in genetics or to learn more about MGfC, please contact us.
Luca’s Legacy – Part Two: The Primacy of Care >

This story is just one example of the groundbreaking efforts taking place at Mass General, home to the largest hospital-based research enterprise in the U.S. — the Mass General Research Institute. The Research Institute encompasses and provides support to thousands of scientists, hundreds of laboratories, and helps to guide, connect and promote this unrivaled community of investigators as they advance the future of medicine, from the bench to the bedside, to the community and world.