If you have a serious health condition, you seek the most effective medical and surgical treatments for the best possible outcomes. But increasing evidence shows that focusing on specific lifestyle factors can also help you heal.
“We focus on how we can break a patient’s goals down into components, which makes it a little bit less overwhelming and helps an individual achieve success.”
The American College of Lifestyle Medicine (ACLM) defines the field as “therapeutic use of evidence-based lifestyle interventions to treat and prevent lifestyle-related diseases in a clinical setting. It empowers individuals with the knowledge and life skills to make effective behavior changes that address the underlying causes of disease.”
Doctors encourage lifestyle strategies for people with various health conditions, including those affecting the heart, nervous system, and joints. These changes typically revolve around six pillars:
- Nutrition
- Physical activity
- Stress management
- Restorative sleep
- Social connection
- Avoidance of risky substances
“Treating the whole person, not just the cancer, is essential in oncology care,” says Amy Comander, MD, a Mass General Brigham Cancer Institute breast oncologist and director of the Lifestyle Medicine Program. “Increasing evidence has demonstrated that, in some cases, focusing on these key lifestyle factors can improve outcomes in cancer and other serious health conditions.”
Six areas to focus cancer lifestyle changes
Dr. Comander and colleagues have launched the Lifestyle Medicine Program to help people with cancer reap the benefits of a holistic approach to care.
“The oncology team wants to ensure that each patient has the tools in place to achieve the best possible outcome,” she explains. “But at the same time, we want to make sure we’re attentive to every aspect of a patient’s health. We ask our patients: How are you sleeping? How are you eating? How are you doing in terms of physical activity and stress management? What kind of social support do you have?”
The program offers individualized consultations about the important role of lifestyle medicine in cancer care. Personalized strategies are important because everyone’s journey is different, and unfortunately, disparities exist in health care. For example, black women who have breast cancer are more likely to experience worse outcomes than white women. Dr. Comander and her colleagues are working to reduce those disparities and support patients at the individual level.
For patients with a diagnosis of breast cancer, the program offers the PAVING the Path to Wellness Program. This is a 12-week introduction to the important role of lifestyle medicine for breast cancer survivors. The goal is to apply evidence-based lifestyle medicine strategies to improve overall health, well-being, and even treatment outcomes.
The Lifestyle Medicine Program consists of a team of experts from across medical specialties. They work together to provide these clinic offerings, as well as in-depth education on specific topics and referrals to specialists. It also offers group visits focused on key topics in lifestyle medicine.
The team helps patients set “SMART” goals: specific, measurable, attainable, relevant, and timely. “We focus on how we can break a patient’s goals down into components, which makes it a little bit less overwhelming and helps an individual achieve success,” Dr. Comander explains.
Managing nutritional concerns with cancer
Having good nutrition and maintaining a healthy weight are essential to maximizing wellness whether you have cancer or not. But if you have cancer, good nutrition also can help you maintain energy, prevent infection, and heal.
Your nutritional needs and priorities are very personal and individualized. A registered dietitian — especially one with extra training or experience in nutrition for people with cancer — can teach you how to use nutrition to achieve or maintain a healthy weight, minimize side effects, and optimize your overall health.
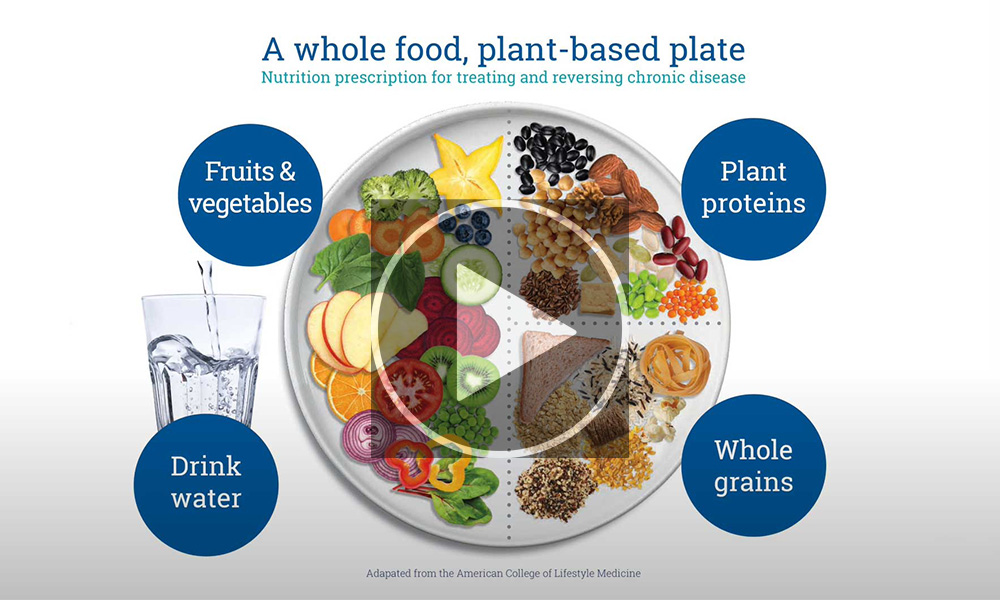
“Increasing research is demonstrating the benefits of a plant-predominant diet, certainly for cancer risk reduction, but also to potentially improve outcomes in certain types of cancer. This diet includes lots of fruits and vegetables and lots of fiber. Recent research has shown that the gut microbiome may play an important role in how a patient’s cancer responds to specific therapies. I think we’ll learn more about this in the next few years,” Dr. Comander says.
The Lifestyle Medicine Program refers patients to individual sessions with registered dieticians through its Nutrition Services. Patients also can attend group Lifestyle Medicine appointments to learn more about nutrition for people with cancer.
Cancer and exercise
There is increasing evidence that exercise has many benefits in people with cancer. Studies show that physical activity during and after cancer treatment can:
- Increase chances of survival from certain types of cancer
- Improve sleep and lessen feelings of fatigue
- Improve quality of life and ability to complete daily activities
- Reduce anxiety and depressive symptoms
- Reduce symptoms of lymphedema (swelling)

Dr. Comander recommends at least 150 minutes of moderate aerobic activity each week, plus strength training twice a week, based on guidance from the American Cancer Society and the American College of Sports Medicine.
Cancer treatment can take a toll on your body and mind. For people who need help starting or sticking with an exercise routine, referrals to physical therapists and community programs can help. A cancer rehabilitation specialist can also work with you during and after treatment to support your ability to function and move better.
To read more about how stress management and restorative sleep can boost your well-being, visit massgeneralbrigham.org.