As recently as the 1990s, experts thought of pediatric patients with bipolar disorder as rare, with mania, depression or attention deficit hyperactivity disorder (ADHD) as explanations for their behavior. But, based on 30 years of clinical work studying hundreds of children with bipolar disorder, Janet Wozniak, MD, has determined it is more common than we think — approximately 15 percent of referrals to the Division of Child and Adolescent Psychiatry at Massachusetts General Hospital are for pediatric bipolar disorder. Dr. Wozniak notes that one-third of adult patients with bipolar disorder developed it before age 12. “Their misdiagnosis as children may have made things much worse for them, as treatments for depression and ADHD, when given to a patient with bipolar disorder, can trigger mania, severe depression or other serious side effects.”
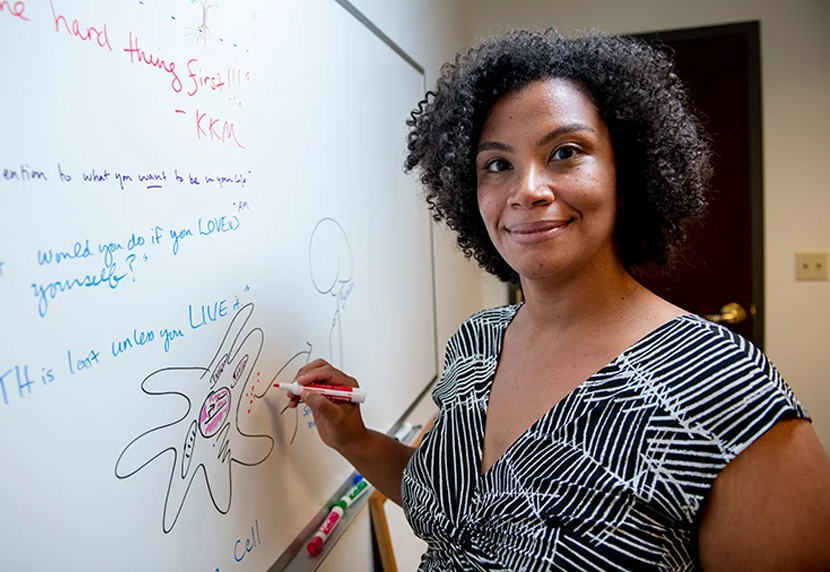
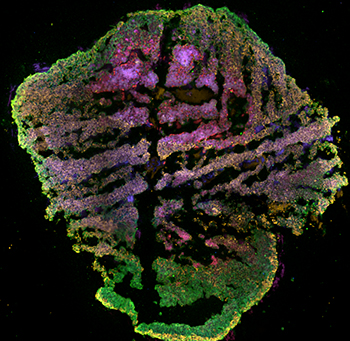
To give pediatric bipolar patients the help they need, Dr. Wozniak has teamed up with Rakesh Karmacharya, MD, PhD, a principal investigator in the Center for Genomic Medicine, on a leading-edge research project, developing and studying brain organoids — mini brains with the same genetic makeup as patients. With funding from the Baszucki Brain Research Fund, Dr. Wozniak and Dr. Karmacharya’s groundbreaking work systematically studies the neurobiology of pediatric bipolar disorder and lays the foundation for precision medicine in child psychiatry.

“Our ultimate goal is to diagnose and treat patients in the early stage of illness. Proper diagnosis is critical since the treatment of bipolar disorder and major depressive disorder are very different, and treating bipolar disorder with antidepressants can make them worse,” says Dr. Karmacharya. Using blood samples collected from Dr. Wozniak’s pediatric-onset bipolar patients, Dr. Karmacharya’s laboratory is creating stem cells to generate patient-specific cerebral organoids, enabling them to study the neurobiological underpinnings of pediatric bipolar disorder.
This information will allow for early and correct diagnosis and set the stage for the development of personalized treatment based on how a specific patient’s brain organoid responds to a particular medication. “Pediatric bipolar disorder starting prior to age 12 affects a significant minority of children — about one to three percent of the population and about 15 percent in our outpatient clinic,” says Dr. Wozniak. “If we could identify this subgroup early and treat them properly, we could prevent the dreaded outcomes of suicide, addiction and criminality. In addition, a better understanding of what has gone wrong in the brain can reduce the stigma associated with bipolar disorder. That would be a tremendous public health achievement.”

Parallel work with adult bipolar disorder is being done at the Dauten Family Center for Bipolar Treatment Innovation at Mass General. Director Andrew Nierenberg, MD, has worked with Paola Arlotta, PhD, at Harvard in developing brain organoids in adult bipolar patients, aimed at exploring the molecular and cellular changes in patients’ brains. “We are growing brain organoids from lithium responders and non-responders to see how those brain organoids change when exposed to lithium — all to try to unlock the mystery of why some people respond and others don’t,” says Dr. Nierenberg.
The Next Frontier in Brain Research
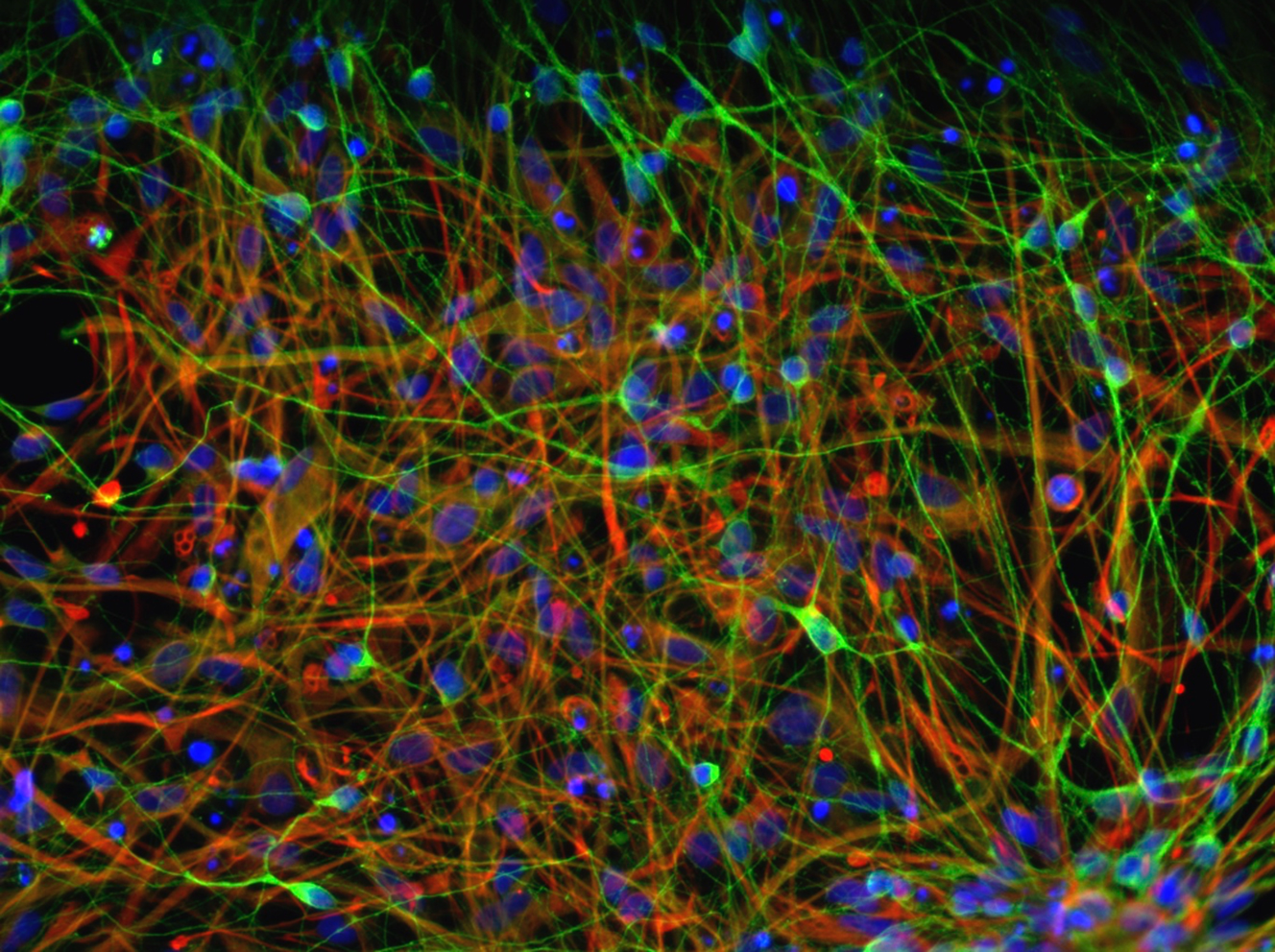
Developing cerebral organoids makes it possible to scientifically investigate the normal trajectory of human neurodevelopment as well as the cellular processes that go awry in pediatric bipolar disorder. To launch this research, Dr. Wozniak recruited her patients to create patient specific stem cells from their own blood, which were then engineered to grow cerebral organoids. Since she has extensive data on their diagnoses, disease trajectories and responses to medications, she and Dr. Karmacharya can systematically link clinical features with cellular findings in the brain organoids to discover disease-specific differences in gene expression, neural firing patterns and response to environmental stress, inflammation and medications.
“Our goal is to take blood from the young patient, make individualized stem cells, generate patient-specific brain organoids and examine if the cellular and molecular characteristics of the brain organoid shows features consistent with bipolar disorder or major depressive disorder. Then, we can make an informed decision about the diagnosis and treatment,” says Dr. Karmacharya.
He also notes there are several medications that can be used to treat bipolar disorder but not all patients respond well to them. Finding the medication that works for one patient often takes months or years. “We can test the different medications in brain organoids of a specific patient and use this personalized medicine approach to decide on the right treatment from the start, eschewing the trial-and-error method,” he says.
The Need — and Opportunity — for Early Intervention
With that objective test, Dr. Wozniak hopes she can recognize at-risk populations and prevent emergence of their bipolar symptoms at a young age. Studies aimed at identifying methods for earlier diagnosis, intervention and more precise, effective treatments for bipolar and other mental disorders are made possible thanks to philanthropic support from generous donors. “If we could identify this disorder with a blood test, we would have the knowledge to administer the correct treatment from the outset which would improve outcomes,” she says. “Understanding the biology of bipolar disorder also reduces the guilt parents feel about their parenting and can encourage them to seek services. Every parent wants the crystal ball to know what’s going to happen in the future. Studies like ours, which bridge the clinic and lab, can help provide that critical information.”
To learn more about how you can support Child and Adolescent Psychiatry at Mass General, please contact us.

This story is just one example of the groundbreaking efforts taking place at Mass General, home to the largest hospital-based research enterprise in the U.S. — the Mass General Research Institute. The Research Institute encompasses and provides support to thousands of scientists, hundreds of laboratories, and helps to guide, connect and promote this unrivaled community of investigators as they advance the future of medicine, from the bench to the bedside, to the community and world.