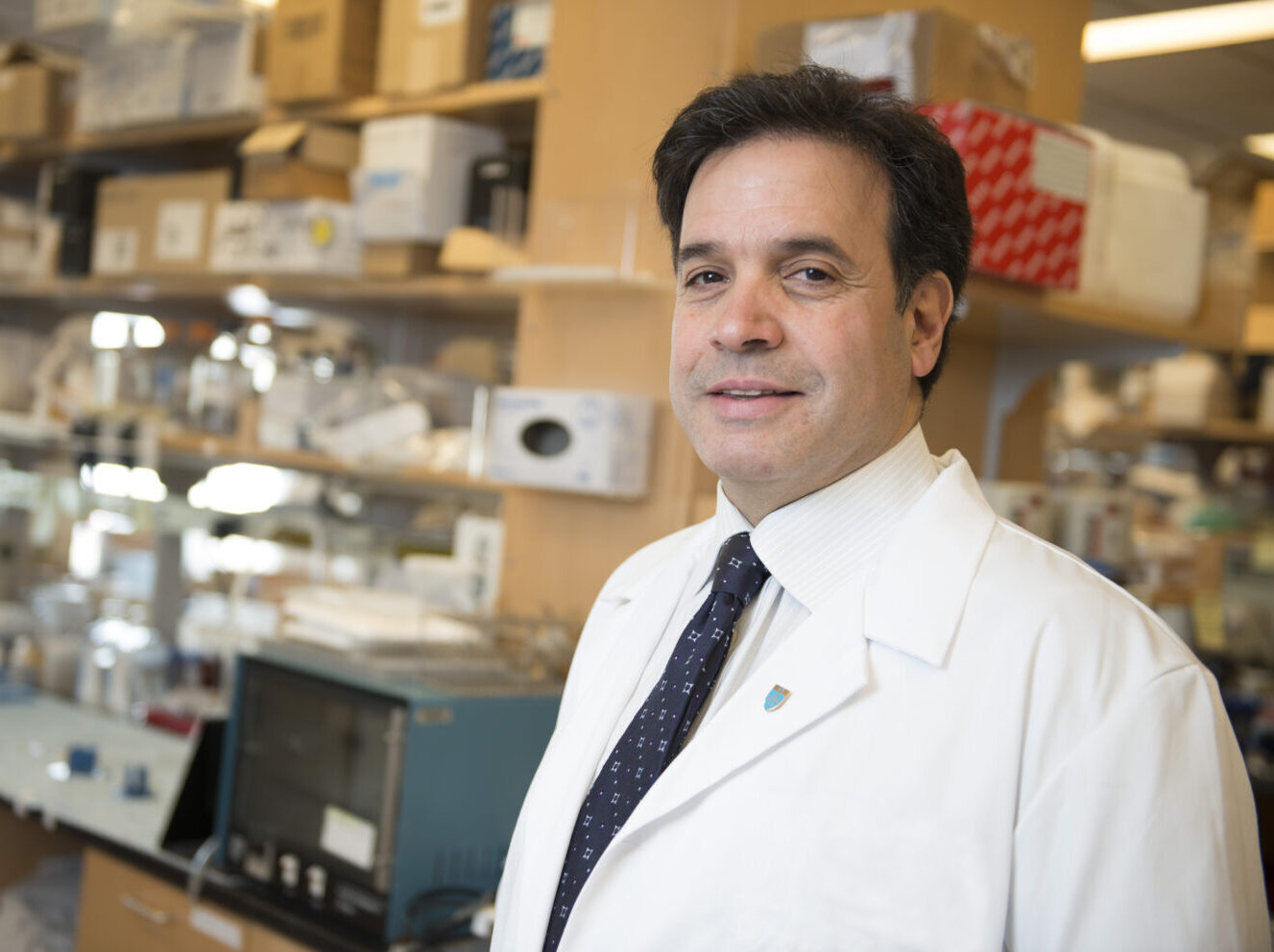
Over the past several decades, research breakthroughs have meant that many of the deadliest age-related diseases — like cancer and heart disease — can be diagnosed and treated early, extending and saving countless lives. Now, thanks to the work of Massachusetts General Hospital‘s Rudolph Tanzi, PhD, the same may soon be possible for another common and complex age-related condition – Alzheimer’s disease. As co-founder and director of the McCance Center for Brain Health, director of Mass General’s Genetics and Aging Research Unit, co-director of Mass General Institute for Neurodegenerative Disease, and the Joseph P. and Rose F. Kennedy Professor of Child Neurology at Harvard Medical School, Dr. Tanzi is helping pioneer a new path for the early intervention and prevention of Alzheimer’s pathology through the Alzheimer’s Disease Clinical Trials Initiative.
Why is early diagnosis so critical when it comes to Alzheimer’s disease?
Alzheimer’s disease typically isn’t diagnosed until the brain has deteriorated to the point of dysfunction. That’s like diagnosing heart disease when the patient already has congestive heart failure. Early detection for Alzheimer’s is increasingly possible, thanks to brain imaging and blood tests that can identify the presence of beta-amyloid — which is to Alzheimer’s what cholesterol is to heart disease. We estimate there are as many as 40 million Americans who are beta-amyloid positive — and, therefore, at high risk of developing dementia, but who don’t yet have any clinical symptoms. It’s great that we can now test for this, but early detection is not enough without safe, effective and affordable therapy options.
How are you trying to solve this problem?
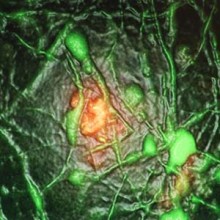
In 2014, my lab developed a cellular model of the disease — Alzheimer’s-in-a-dish, if you will. We can fit 106 of these tiny organoid models on a plate and watch each one play out the entire 30-year process of Alzheimer’s in just six weeks. It’s made drug discovery 100 times faster, 100 times cheaper — and this model has become the basis for the McCance Center’s Alzheimer’s Disease Clinical Trial Initiative. Over the past seven years, instead of testing one drug at a time in mice, we’ve used the organoid model to observe the effects of nearly 1,800 drugs that are already FDA-approved for other uses, as well as nutritional supplements and combinations of drugs and supplements. The idea was to ask only one question: What are we seeing in the dish? Which ones stopped the amyloid? In doing so, we’ve identified more than 50 combinations of safe drugs that dramatically reduce Alzheimer’s pathology in our brain organoid models.
What’s the next step?
Now that we know what works, and what is safe because they are already FDA-approved, our next step is to move these novel combinations into human clinical trials. These clinical trials, which we’re funding through philanthropy, are designed to be simple and efficient. We’re not trying to improve cognition right away — we want to see if what we saw in the dish is replicated in the patient. Because we can track beta-amyloid in the blood, it will show us if the drug is getting into the brain, and if it’s reducing pathology. If one of the combinations is successful, we can hand it off to a pharma company to develop. We’ve done our work, and shown the pitcher has promise, so now it’s off to the big leagues.
To learn more about how you can support Dr. Tanzi and research in Alzheimer’s disease, contact us.