When a blood clot travels to the lungs it can cause a pulmonary embolism (PE), a dangerous condition that affects an estimated 800,000 Americans annually and kills about a quarter of them, especially if left untreated. That figure far outstrips U.S. fatalities from traffic accidents, HIV and breast cancer combined, and the number is rising, mostly because of an aging population who are more at risk.
“Pulmonary embolism is underrecognized, undertreated and undermanaged,” says Kenneth Rosenfield, MD, of Mass General.
“Pulmonary embolism is underrecognized, undertreated and undermanaged,” says Kenneth Rosenfield, MD, an interventional cardiologist and vascular specialist at Massachusetts General Hospital. Teams at Mass General and around the globe have been looking for ways to more effectively treat PE, and the good news is that some new models show great promise. The not-so-great news is that what works may not be easy to implement, at least in the near future.
Treating this condition effectively can require quick, interdisciplinary thinking. A radiologist may be needed to pinpoint the damage, and coming up with a plan for treatment may call for a skilled cardiologist or an expert in vascular or pulmonary medicine — and often a surgeon to remove the blockage. Yet that kind of cooperation doesn’t always come together smoothly. A patient, or a patient’s data, may be shuttled from one place to another as various specialists consider a case, all while the clock is ticking.
Pulmonary Embolism Response Team
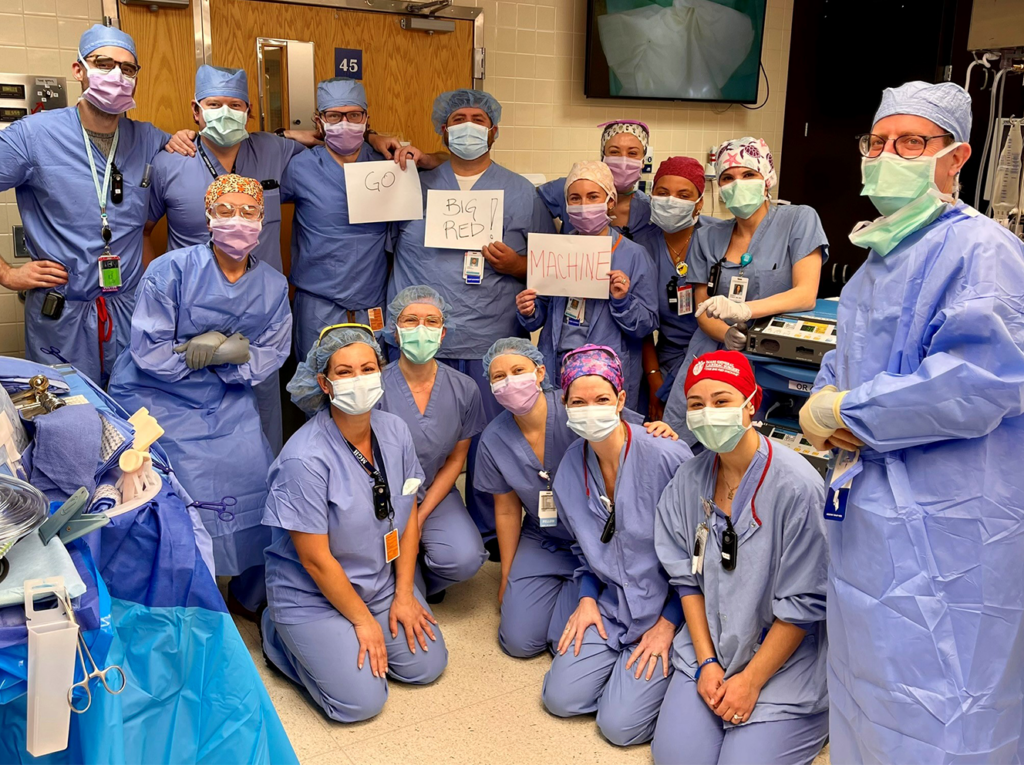
In 2012, to create a better way to evaluate and treat patients, Dr. Rosenfield and several colleagues at Mass General developed and launched the first pulmonary embolism response team (PERT) program in the United States. With this treatment approach, when an embolism is discovered, an alert immediately goes out to notify a dozen or more specialists, who convene for a virtual meeting to map a treatment plan. Since the introduction of PERT, mortality for Mass General patients with massive pulmonary embolisms fell to less than half the national average.

During the past six years, more than 150 other hospitals — not only large academic medical centers and smaller community hospitals, but also international hospitals as far away as China — have also embraced a team approach to treating pulmonary embolisms. More than 80 of those institutions recently combined to launch the PERT Consortium, adopting the acronym that Dr. Rosenfield and his colleagues used to describe their multidisciplinary model of care.
“One of the biggest factors motivating people to join the PERT Consortium is the ability to join a consortium-wide registry made up of data from all PERTs,” says Dr. Rosenfield. “That will empower institutions to benchmark their performance and their quality of PE care against that of others around the country.”
A Question of Continued Momentum
But whether this momentum will continue to build is subject to other factors. Some hospitals find the staffing demands of the program beyond their reach. Robert Maholic, DO, an interventional cardiologist affiliated with UPMC Hamot in Erie, Penn., describes the challenge: “We don’t have a dozen different specialists on call because we don’t have a large staff. In terms of scale, Mass General’s PERT model is intimidating to emulate.” PERT surveys so far have shown that most existing PE teams involve four specialties, and fewer at smaller hospitals with lower numbers of physicians on staff. Yet even at this smaller size, says Dr. Maholic, UPMC has seen remarkable success. “I advise smaller hospitals that a PE team can be minimal, two or more specialists.”
A larger obstacle may be a lack of remuneration for many PERT services. “Not everyone is able to bill when multiple physicians are involved,” says Jay Giri, MD, MPH, a cardiologist at the Hospital of the University of Pennsylvania and founder of the PERT program there. Moreover, hospital administrators are reluctant to dedicate money or physicians to a team model that is still considered experimental. But despite these complications, “the concept of PERT is here to stay,” Dr. Rosenfield emphasizes. “It may take different forms, though, and each hospital will be unique.”
Demonstrating Benefits
So far, there have been only three published reviews of PERT implementations, including the one at Mass General. According to Dr. Giri, some critics have complained that the team approach unnecessarily complicates treatment, involving more specialists than are needed to provide effective care. Moreover, the type of collaboration among specialists that PERT requires is sometimes problematic. All the physicians involved must contribute their own expertise and perspectives while also putting the team’s goals above self-interest. “At some hospitals, egos, territoriality and self-protection do get in the way,” explains Dr. Rosenfield.
For PERT to gain wider acceptance, additional outcomes research on outcomes will need to demonstrate its benefits, says Jaafer Golzar, MD, a cardiologist with Advocate Health Care in Oak Lawn, Ill. “We need data to show we’re saving lives,” says Dr. Golzar, who helped launch pulmonary embolism teams at two hospitals in the system. Yet while he has only anecdotal evidence that care has indeed improved with this approach, he is convinced of its value. “Recognizing higher-risk patients and treating them with advanced therapies is so important,” Dr. Golzar says. “A multidisciplinary team model has made that much more efficient.”
To learn more about supporting cardiovascular care and research at Mass General, please contact us.
This story was first published by Proto Magazine.