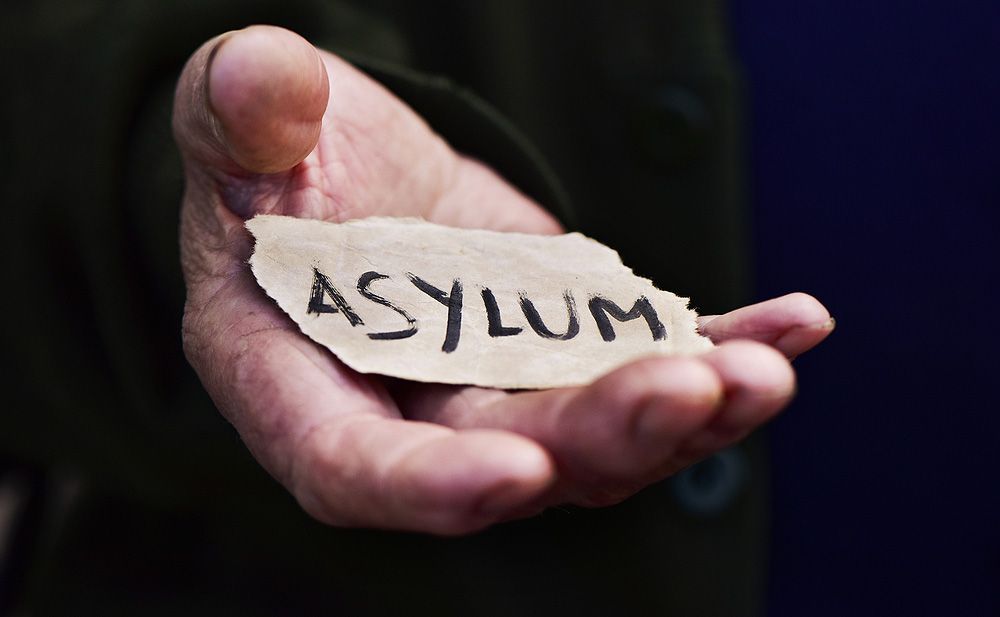
For refugees who have fled violence and persecution in their home countries, attaining asylum status in the United States can be a beacon of hope at the end of a long, dark tunnel.
Asylum is a permanent residency status granted by the government to individuals who have experienced violence and persecution (such as torture or sexual assault) in their home countries, or who believe they will be subject to violence and persecution if they return.

Attaining asylum is not an easy process, however.
Navigating a Challenge
The immigration system can be challenging to navigate, particularly for those who do not speak English as a first language, or have a fear of government organizations due to their uncertain legal status. It can also be difficult to prove claims of past physical and mental abuse, particularly if the incidents occurred thousands of miles away.
A team of clinicians from Massachusetts General Hospital is working to help this vulnerable population through the MGH Asylum Clinic. Clinic members volunteer their time to provide independent medical assessments of individuals seeking asylum based on a past history of physical or mental abuse.
The team meets twice a month to provide the assessments, which are typically arranged through connections with a network of immigration lawyers and community support groups. Patients are from across New England and most receive their primary medical care outside of Mass General.
“We must also consider the legal status of our patients as a social determinant of health…”
“As physicians, we listen to their stories, perform physical examinations to corroborate those stories, and submit an affidavit to the court with an objective assessment of whether our findings are consistent with the reported abuse,” explains Matthew Gartland, MD, director of the MGH Asylum Clinic.
From Concept to Reality
The concept for the clinic originated with Eleanor Emery, MD, who recently completed her residency in Internal Medicine at Mass General. Dr. Emery helped to start a similar clinic while studying at Weill Cornell Medical School.
Team members received training from Physicians for Human Rights, which provides a legal background on the qualifications for asylum and a foundation in medical forensic examination that is specific to the types of trauma experienced by immigrants applying for asylum.
In addition to providing independent medical assessments, the team is also making connections with local immigration advocacy groups, who help in connecting Mass General patients to legal services as the first step in the asylum process.

Volunteering at the clinic has been a natural fit for Jo Henderson-Frost, MD, an Internal Medicine resident at MGH Chelsea, where more than half of patients are foreign-born, many from Central America.
“In the primary care clinic, we often hear stories of trauma and refer patients to mental health specialists, but we must also consider the legal status of our patients as a social determinant of health, and ensure they have access to legal representation,” Dr. Henderson-Frost says.
The Hidden Signs of Trauma
The stories that clinic members hear in their evaluations can be heartbreaking, though the team members find some comfort in being able to bear witness to the stories and help refugees strengthen their case for asylum.
During a recent evaluation of a young mother seeking asylum, Drs. Gartland and Henderson-Frost learned about the political and gang violence she faced in her home country, as well as a sexual assault she suffered during her journey to the United States.
“These are the stories of our patients and our neighbors. They are difficult for patients to relive and often difficult to hear.”
Following a period of detention at the border, the woman was released pending a hearing in Immigration Court. In Boston, she has found a new life — joining a church, finding a job, and starting a family. Her future in the United States has remained in jeopardy, however. She lives in constant fear of deportation and the consequences of returning to the place she fled.
In clinic that day, the woman’s story all unfolded while her two-year-old daughter was running in and out of the room, oblivious to the traumatic subject matter being discussed.
“These are the stories of our patients and our neighbors. They are difficult for patients to relive and often difficult to hear,” Dr. Gartland says. “If we educate ourselves, create an open environment and support patients to process life after trauma, we can have an incredible impact on people’s lives.”
Funding for the Future
While the clinic is powered by volunteers, Dr. Gartland hopes to find funding to support administrative expenses and cover the cost of additional training sessions to bring more clinicians onto the team.
“Almost every time I speak about the clinic, someone comes up to me afterwards to say they would love to get involved.”
To learn more about the MGH Asylum Clinic, please contact Dr. Gartland.