The prevalence and severity of mental health concerns have reached crisis levels across our country and the globe, profoundly and uniquely affecting our children, adolescents and college-aged youth. Anecdotally, we know that the pandemic, the threat of school gun violence and the daily stressors children and adolescents face at home, school and on social media have disrupted the health and stability of families on nearly every level. And the data supports it.
The shortage of mental health providers makes this problem significantly more dire. Approximately 15 million children and adolescents need mental health support, but there are only approximately 9,000 practicing clinicians in the U.S. qualified to care for young people, and many of those do not accept insurance.
Massachusetts General Hospital is making concerted efforts to address these important and urgent mental health needs through unique, scalable, evidence-based programs that expand access to youth mental health care.
The Resilience and Prevention Program
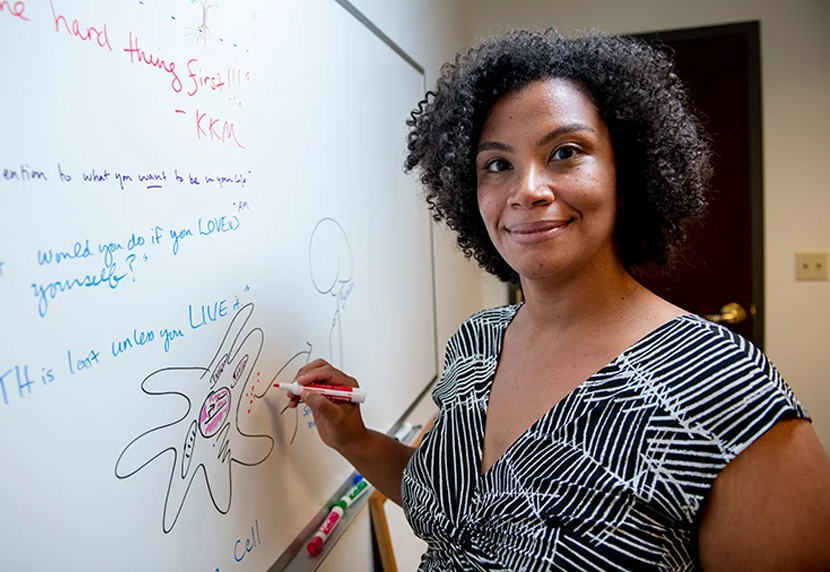
Since 2012, Daphne Holt, MD, PhD, founder and director of the Resilience and Prevention Program at Mass General, has been working with at-risk young people from adolescence through college age, leveraging programs that seek to build emotional resilience and prevent the development of disabling mental illnesses, including depression, suicidality, anxiety and psychosis. Her group-based interventions for middle school, high school and college-age young people are highly scalable since they are effective when delivered in-person, in a school or community setting, or virtually via video conferencing or virtual reality technology.
“These group interventions for at-risk adolescents and young adults have shown promising outcomes in reducing depression, suicidal thinking and other symptoms of emerging mental health conditions, and positive improvements in day-to-day functioning, academic performance and engagement in school and community,” says Dr. Holt. “Resiliency skills can also reduce the impact of a mental health issue if one does develop.”

Think:Kids Program
The Think:Kids program uses a research-based, trauma-informed approach called Collaborative Problem Solving® (CPS) to help children with behavioral health challenges. This highly effective approach shows families, professionals and organizations how to teach kids the neurocognitive skills they need — including problem solving, flexibility and managing frustration — to navigate the world around them. Think:Kids has certified CPS trainers across North America, the UK and Australia, delivering services in therapeutic settings, correctional facilities, child welfare organizations, parenting classes, primary care facilities and schools.
The program can also be adapted so trainers can respond to the unique culture and needs of each community. “The skills related to resiliency need to be practiced in natural environments,” says founder and director J. Stuart Ablon, PhD. Think:Kids relies on philanthropy to expand and scale their work and experiment with novel ways of delivering the model so it remains accessible and affordable to all.

PRIDE Treatment Program
Luana Marques, PhD, Phyllis and Jerome Lyle Rappaport MGH Research Scholar 2020-2025 and founder and director of the Community Psychiatry Program for Research in Implementation and Dissemination of Evidence-based (PRIDE) Treatments at Mass General, knows that every child can benefit from growing their resilience and problem solving skills. “Everyone deserves to learn the resilience enhancing skills needed to potentially change the trajectory of their lives,” she says. The PRIDE program aims to increase access to quality mental health care among underserved populations, where quality care and best practices can be less accessible. Since 2013, the program has partnered with community organizations to provide assessment, training, coaching, consultation and continuous evaluation of state-of-the-art cognitive-behavioral strategies that are designed to be delivered by youth development professionals to maximize accessibility.

Child Resiliency Program
The Child Resiliency Program (CRP) includes mindfulness and behavioral interventions that serve the mind and the body. The research-validated stress management program draws from evidence-based interventions to manage stress and build resilience in children, adolescents and young adults. The program integrates mindfulness and coping skills with cognitive behavioral-based skills that are developmentally modified for kids of all ages. The program also engages parents and educates and supervises paraprofessionals who work with CRP patients. The CRP works closely with the Benson Henry Institute (BHI) for Mind Body Medicine, which seeks to further understand mind body medicine, to provide treatment that reduces the physical and emotional impact of stress and to train health care professionals, medical students, post-doctoral fellows and educators. “Children suffer the effects of stress much like adults,” says BHI Director, Gregory L. Fricchione, MD. “But children must also face their special developmental challenges.”

Resilient Youth Program
Since 1989, the CRP and BHI have collaborated with clinicians, educators and outside organizations to provide the Resilient Youth (RY) program. The RY program was founded by BHI founders Herbert Benson, MD, and his wife, Marilyn Wilcher, who recognized that childhood is a pivotal time to teach young people stress management resiliency skills to provide a livelong skill set for managing stress and enhancing wellbeing. The program is delivered in group settings and offers training to clinicians, educators, parents, guardians and community stakeholders who support kids, ultimately expanding access to care for youth in need.
Based on the clinical programs of the BHI, the Resilient Youth curriculum was reformatted in 2020 to meet the needs of 21st century students, educators and families. “The program has established itself as a game-changer for the well-being of kids and is inspiring a long overdue shift to prevention and early intervention, increasing access for youth,” says Tim Wilens, MD, Chief of the Division of Child and Adolescent Psychiatry. “Our research shows that at the end of 12 weeks, there is a clinically and statistically significant improvement in parent and youth outcomes.”
To learn more about how you can support Pediatric Psychiatry at Mass General, please contact us.