Massachusetts General Hospital’s David Lin, MD, is changing the way we think about recovery from stroke.
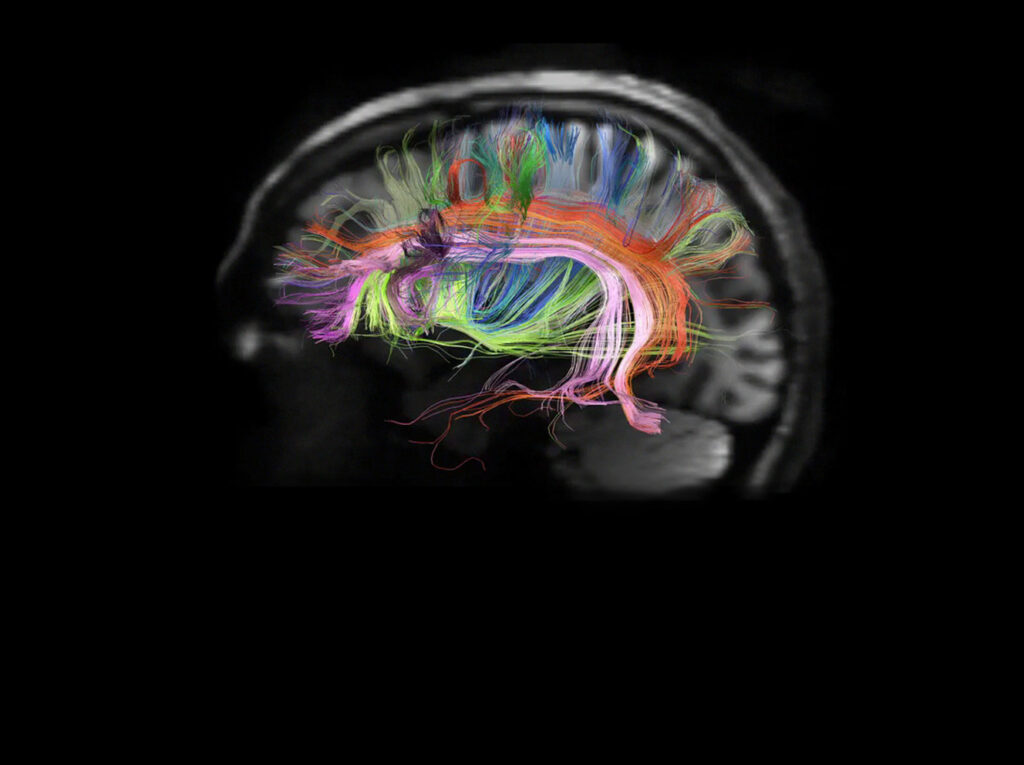
“Post-stroke recovery has traditionally been guided by physical rehabilitation,” says Dr. Lin, a critical care neurologist, neurorehabilitation specialist and Director of the NeuroRecovery Clinic at Massachusetts General Hospital. “In order to have new and major breakthroughs, though, we need to better understand the neuroanatomy and physiology underlying movement.”
In a paper published in the journal Neurology in May 2023, Dr. Lin’s team shares results of their project to begin mapping specific patterns of paralysis to specific parts of the brain with the goal of focusing occupational and physical therapy with greater precision to drive recovery after stroke.
For Mass General stroke patient John Didier, Senior Director at Dell EMC, participating in Dr. Lin’s StrokeMotor Rehabilitation and Recovery sTudy (SMaHRT) provided him with the guidance and encouragement he needs.
Stimulating Motor Neurons Helps With Repair
Five years ago, John, 56, experienced an acute ischemic stroke — the most common type of stroke, it happens when a blood vessel in the brain is blocked by a blood clot or a buildup of fatty deposit and cholesterol — that left him with limited mobility on much of his left side.
After spending time in the Milford Hospital ICU, cardiologists repaired the cause of the stroke — patent foramen ovale (a hole in John’s heart) — and he was transferred to a rehabilitation hospital for five weeks before going home in a wheelchair. He continued occupational and physical therapy on his own, since his left side was still significantly impacted: he walked with a cane and had no use of his left hand.
“After a stroke, a significant amount of uncertainty exists,” John says. “After all the initial tests, visits and inpatient therapy, care and support drops off a cliff. While I continued to see a neurologist and other doctors, the frequency was only once or twice per year.”
“Post-stroke care is a long journey,” says Dr. Lin, “and we need to more accurately track who recovers motor function, who doesn’t — and how we can stimulate motor neurons to encourage repair.”

Participation in Clinical Study Motivated Continued Rehabilitation
“I’m very motivated, and I tried to continue physical therapy on my own hoping I was doing the right things,” John says. “But I had very little guidance on how to maximize my recovery.”
When Dr. Lin invited him to participate in the SMaHRT study at Mass General, a longitudinal study focused on understanding patterns of recovery, John did not hesitate.
John says that participation in the study served as another form of therapy. “It gave me an outlet for questions, feedback, new therapies and the feeling of being part of something important that will help other stroke victims in the future,” he says.
The SMaHrt study emerges from Dr. Lin’s Laboratory for Translational Neurorecovery (LTNr), which is working on transforming stroke rehabilitation by advancing our understanding of brain mechanisms that enable stroke recovery. The lab uses a variety of techniques — rehabilitation robotics, magnetic resonance imaging, electroencephalogram, near-infrared spectroscopy and transcranial magnetic stimulation — to understand and improve hand and arm movement after stroke.
Long-term Study Reveals Areas of Brain Where Damage Occurred
“Following the study participants over time, using the information to guide occupational therapies more precisely to the area of the brain damaged by the stroke, and then measuring progress has had a profoundly positive impact on our patients,” says Dr. Lin. “While this study is focused on motor skills in the hand and arm, with philanthropic support, we hope to train more neurologists to take this approach to stroke recovery so that we can provide our patients with the best possible rehabilitation path.”
John says his recovery has been slow, but participating in the trial has been a huge boost.
“Regaining function is like learning a new language,” he says. “First you have to create patterns, and then build on them. But I have regained a lot of movement in my left hand and arm and am now walking three miles a day. I don’t think that would have happened without the support of Dr. Lin and his team.”
To learn more about how you can help advance neurorecovery research and improve post-stroke recovery, please contact us.
I have regained a lot of movement in my left hand and arm and am now walking three miles a day. I don’t think that would have happened without the support of Dr. Lin and his team.