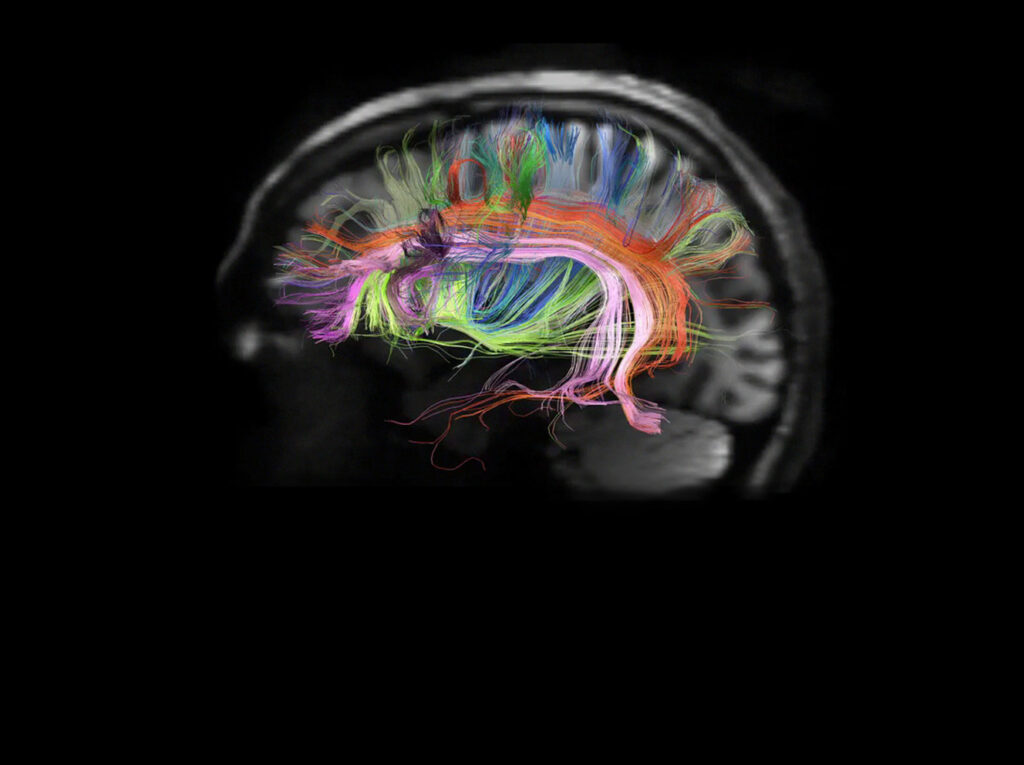
The human brain is a three-pound bundle suspended in fluid and covered with a bone helmet; a dazzling network of 86 billion cells transmitting an ever-shifting pattern of electrical signals across a web with trillions of junctions. Complex, constantly in flux, hard to access, our brains have a knack for keeping secrets — especially when it comes to the diseases that afflict them.

Much of what we know about the biology of psychiatric and neurological disease has been discovered studying the brains of people who died. But postmortem tissue has a major drawback: It only shows the final stage of the disease, not how it developed.
Mouse models — which have allowed scientists to observe the progression of diseases like cancer and diabetes — haven’t been able to capture the genetic, cellular and behavioral complexity of the human brain. But a new modeling technique is giving researchers and clinicians across Massachusetts General Hospital an unprecedented glimpse at how brain diseases like schizophrenia and dementia develop. And it starts with a biopsy.
Brain Disease and Cell Networks
Using skin cells donated by patients and volunteers, Mass General scientists are now able to grow tiny networks of brain cells in lab dishes, networks that reproduce the precise genetic characteristics of the person from whom they were taken. And these innovative models make it possible to observe new disease mechanisms, identify potential drug targets and develop new therapeutic approaches that could ease the global burden of brain disease and transform the lives of millions.
Since its founding in 1811, Mass General has been at the forefront of medical innovation. Our physicians, researchers, nurses and other staff are committed to making bold breakthroughs that provide revolutionary results for patients. The Mass General Research Institute promotes, supports and guides the largest hospital-based research program in the United States. As fresh insights and new technologies emerge, such discoveries often evolve in powerful and unexpected ways.
“For liver disease or cancer, you can easily get a biopsy. That isn’t an option with psychiatric patients.”
Pressing ‘Play’ with Stem Cells
The sorts of research models now being deployed against brain disease are not a new idea. As far back as the 1950s, researchers in cancer were using cells grown from patients to study disease progression and test treatments. But brain disease proved far more difficult to reproduce in the lab.
“One of the great challenges of psychiatry is that we can’t access the tissue we care most about until the patient has died,” says Roy Perlis, MD, a psychiatrist and the director of the Center for Experimental Drugs and Diagnostics in Mass General’s Center for Genomic Medicine. “For liver disease or cancer, you can easily get a biopsy. That isn’t an option with psychiatric patients.”
The advent of stem cell technology changed everything. Stem cells are special, self-renewing cells capable of generating any of the hundreds of types of cells in the human body. In recent years, researchers have figured out a way to harness that special capacity.

By introducing certain genes, scientists can produce proteins into mature cells and turn back the developmental clock, transforming them into stem cells. These new, “reprogrammed” stem cells can be further engineered in the lab to become neurons and glia, the building blocks of the brain.
Placed in a lab dish, these neurons mature over time and form networks, just as they would in the brain. Best of all, because these microscopic model systems are genetic replicas of the donor, the neurons can in a number of cases develop the same disease features.
“Patient-derived models give us the ability to press “play” and watch the earliest stages of brain disease develop in a way we never could before,” says Stephen Haggarty, PhD, Stuart and Suzanne Steele MGH Research Scholar 2017-2022, director of the Chemical Neurobiology Laboratory in the Mass General Center for Genomic Medicine.
A New Window on Disease Biology
A decade ago, when genomic medicine was in its infancy, many in the scientific community believed that major psychiatric diseases, like schizophrenia and bipolar disorder, might be caused by just a handful of faulty genes. They quickly realized they were wrong. Genomic studies implicated dozens and in some cases hundreds of genes that play a role in causing these devastating diseases.
“Our goal with these models is to shift the focus of research from treating symptoms to prevention.”
“It was like we’d been hiking a mountain, and thinking we’d reached the top, only to see another peak towering ahead of us,” Dr. Perlis says. He and others at Mass General needed a better way to select the most promising genes to pursue. They decided to try growing neurons in the lab using cells taken from patients.
“At the time that we started, in 2009, it was just a vision,” Dr. Perlis says. “It seemed like the best way to understand how all these genes were working together to contribute to a disease.” Because the skin provided an easy source of mature cells, Dr. Perlis learned how to perform a skin biopsy and started collecting samples.
Today, thanks to Dr. Perlis and other visionary minds, the Mass General Neuro Bank houses one of the world’s largest collection of stem cells from patients with psychiatric disease. The collection includes unique samples from more than 400 patients and healthy volunteers, each linked to detailed clinical data and cognitive testing. It has enabled researchers from Mass General and elsewhere to create patient-derived models of a wide range of psychiatric conditions. And the observations they are making may shape the future of care for brain disease.

Seeing Brain Disease in Real Time
In early 2019, Dr. Perlis and his team used patient-derived models of schizophrenia to observe synaptic pruning, a normal part of the developmental process during adolescence, where immune cells remove unnecessary connections between brain cells. Genomic studies, and later mouse models, had suggested that excessive synaptic pruning played a primary role in schizophrenia, but it had never been explored in human brain cell models. The Mass General team was able to observe the process in a patient-derived model and build on earlier findings from mouse models.
“Now that we can model excessive pruning in schizophrenia, we can use that model to test potential treatments,” says Dr. Perlis. An additional benefit of personalized cell models is that they can be grown in massive numbers — allowing them to be screened against libraries of existing drug compounds. One such screen performed by Dr. Perlis and the team found that exposure to a common antibiotic could slow, and sometimes stop excessive synaptic pruning.
“Having parallel roles as a scientist and a psychiatrist gives me a more nuanced perspective …”
“Our goal with these models is to shift the focus of research from treating symptoms to prevention,” Dr. Perlis says. “And so, while it’s only a preliminary finding, it is promising and a step in the right direction.”
For Rakesh Karmacharya, MD, PhD, a psychiatrist and faculty member in the Mass General Center for Genomic Medicine, patient-based models are an invaluable guide in the lab and clinic.
“A lot of people who study the biology of schizophrenia or bipolar disorder have never seen a patient,” Dr. Karmacharya says. In the clinic, Dr. Karmacharya treats schizophrenia and bipolar disorder patients presenting with their first episodes of psychosis. In the lab, he studies three-dimensional brain organoids generated from the stem cells that he makes from these patients. These complex brain models reproduce many aspects of brain development and organization and provide novel and unique ways to interrogate the biology of the disease affecting his patients.

“Here at Mass General, I’m able to study the complex neurobiology of the disease using brain organoids that we make from patients I see in the clinic,” he says. “Having parallel roles as a scientist and a psychiatrist gives me a more nuanced perspective and enables me to ask questions that are most relevant clinically and scientifically.”
Testing New Therapies
In 2013, Dr. Haggarty, a chemical biologist specializing in the development of new therapeutics for brain disease, approached his colleague, behavioral neurologist Brad Dickerson, MD, about creating a personalized cell model of a patient with frontotemporal dementia (FTD).
The most common form of dementia for people under 60, FTD destroys the nerve centers in the brain that govern personality, language and emotion. As with Alzheimer’s, a related form of dementia, there is no known treatment for FTD.
Dr. Haggarty had an interest in targeting tau, the toxic protein believed to cause FTD and Alzheimer’s. Dr. Dickerson had been collecting skin cells from patients as part of a long-running study of FTD in families. Together, the two and their teams spent more than three years in the lab refining the first personalized cell model of FTD.
Dr. Haggarty is convinced that such a groundbreaking collaboration on a complex brain disease could only happen at a place like Mass General.
“This is as genetically accurate a model of the disease as we can get,” Dr. Haggarty says. The new model is already yielding revolutionary results. Earlier this year, his team used the patient-derived model to test an experimental technique for clearing tau from brain cells. The technique is now in development as a drug, and Dr. Haggarty believes it has potential to treat other neurodegenerative conditions, including Parkinson’s disease, amyotrophic lateral sclerosis (ALS) and Huntington’s disease.
Dr. Dickerson believes that additional models, possibly derived from members of the same family, may one day help reveal features that indicate the onset of FTD before a patient is symptomatic. “In some cases, you have a parent and child who carry the same mutation for the disease, but it develops at different times in their lives,” he says. “But if we could the identify genetic markers that make them different, we might one day be able to use those markers to unlock the cellular chemistry — and therefore potential medicines — to delay or even prevent FTD.”
For his part, Dr. Haggarty is convinced that such a groundbreaking collaboration on a complex brain disease could only happen at a place like Mass General. “As a chemical biologist at Mass General, I work alongside experts in imaging, genetics, and patient care,” he says. “We are so fortunate to have the kind of environment and the resources that can catalyze those interdisciplinary interactions.”
To learn more about how you can support the Center for Genomic Medicine, please contact us.
To find out how your support can advance the work of the Department of Psychiatry, please contact us.