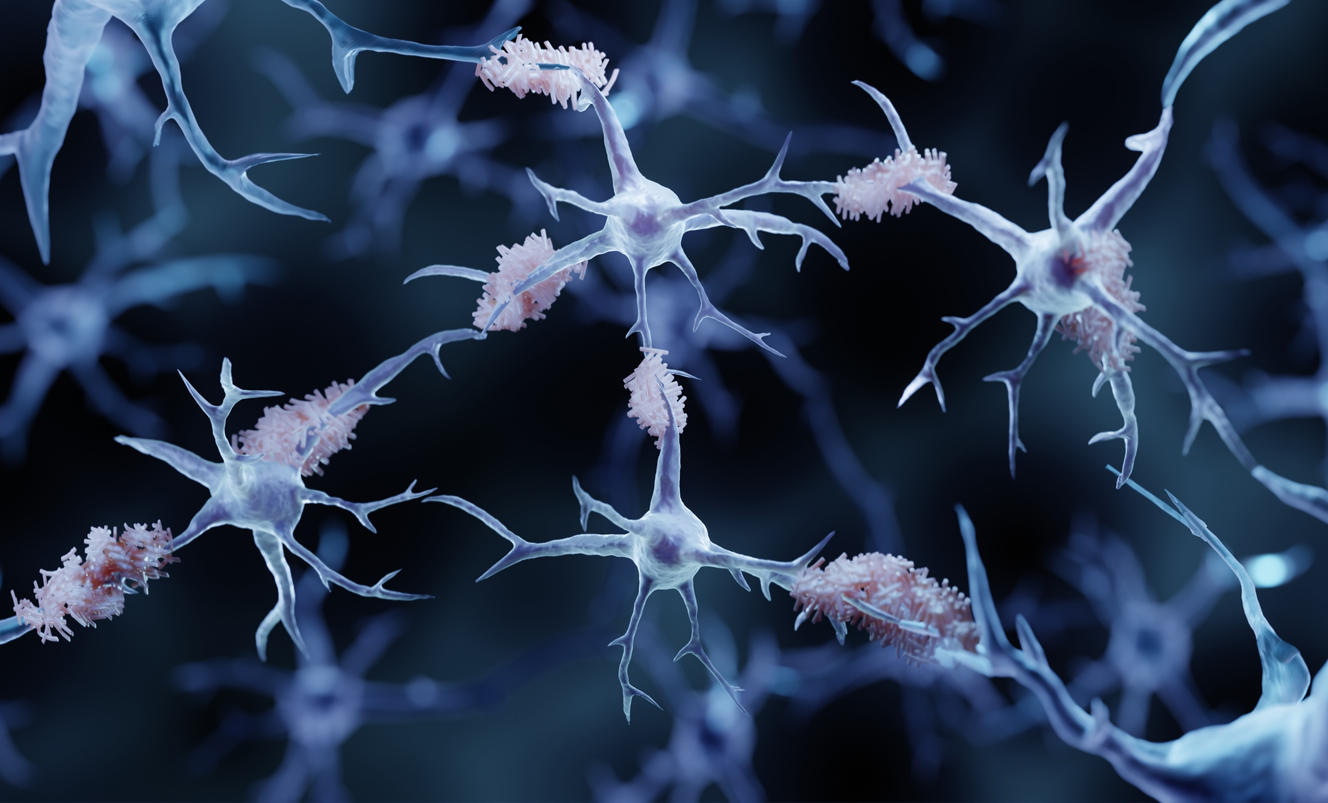
With as many as 40 million Americans already living with amyloid plaques and tau tangles in their brains — placing them at high-risk for Alzheimer’s disease and related dementias — Massachusetts General Hospital clinicians and scientists are urgently accelerating the development of promising treatments.
As chief of the Memory Division in the Neurology Department at Mass General, Teresa Gomez-Isla, MD, PhD, works closely with individuals living with Alzheimer’s disease. Dr. Gomez-Isla oversees a team that cares for more than a thousand patients each year, and as principal investigator of an Alzheimer’s Research Laboratory in the MassGeneral Institute for Neurodegenerative Disease, she leads groundbreaking studies around the molecular underpinnings of the disease as well as research efforts in the Massachusetts Alzheimer’s Disease Research Center (ADRC) based at Mass General.

A New Option to Slow the Disease
“We are using our data to identify people at risk and develop improved therapies to preserve cognition for everyone.”
Almost immediately after last year’s FDA approval of lecanemab for people with early-stage Alzheimer’s, Dr. Gomez-Isla used philanthropic support to launch the Alzheimer Therapeutic Program across Mass General Brigham to quickly screen patients and determine if they qualify for the drug, and to monitor qualified patients to track side effects over time and provide support as needed.
“Lecanemab marks an exciting step forward in our understanding of the biology of this disease,” says Dr. Gomez-Isla. “It slows disease progression in some patients, while providing us with valuable information that will help us develop and tailor therapies to stop the disease, repair the damage and prevent it entirely.”
At the same time, Dr. Gomez-Isla pursues her research into understanding how some resilient brains fend off Alzheimer’s despite the accumulation of plaques and tangles that are hallmarks of the disease.
“We are using our data to identify people at risk and develop improved therapies to preserve cognition for everyone,” Dr. Gomez-Isla says. “We are encouraged by new blood biomarkers that allow us to see who already has Alzheimer’s brain pathology (beta-amyloid plaques, tau-tangles and neuroinflammation) even before they have any cognitive symptoms. Early detection and early treatment are critical to reducing the toll this disease takes on so many.”
A Deeper Understanding
Steven Arnold, MD, sees patients with Alzheimer’s and related dementias. He also serves as managing director of the Interdisciplinary Brain Center at Mass General and leads the Biomarker Core Laboratory at the ADRC. His work moves our understanding of each person’s Alzheimer’s disease beyond amyloid plaques and tau tangles to characterize the varying contributions of inflammation, vascular, metabolic and other factors that drive cognitive decline. With a deeper understanding of the factors driving one person’s illness compared to another’s, he hopes to implement more effective treatment tailored to the individual, and then ensure that it is working.

“With participants serving as their own controls, SEED overcomes the challenge of disease variability among participants in conventional clinical trials, with the additional benefit of welcoming the participation of diverse and often underrepresented people in research.”
His innovative approach, Single-Case Early-Phase Experimental Design (SEED) trials, tests each person against themselves — asking the simple question, “Does one specific patient benefit from a particular intervention?” SEED trial designs are flexible. They precisely measure a treatment’s effects in small numbers of patients in short order to determine if it helps — and, if so, to understand what it was about that person that corresponded with that response.
“With participants serving as their own controls, SEED overcomes the challenge of disease variability among participants in conventional clinical trials, with the additional benefit of welcoming the participation of diverse and often underrepresented people in research,” Dr. Arnold says.
The Promise of “Alzheimer’s-in-a-Dish”
While Drs. Gomez-Isla and Arnold care for patients, researcher Rudolph Tanzi, PhD, director of both the McCance Center for Brain Health and the Genetics and Aging Research Unit at Mass General, works in the lab, screening drugs with a revolutionary human brain organoid model called “Alzheimer’s-in-a-Dish.”
With this astonishingly efficient tool, he and his team have already screened 1,700 drugs approved by the FDA for other uses (meaning they have already been deemed safe for humans) as well as thousands of natural products. More than 250 showed great promise for their ability to slow or stop Alzheimer’s disease.

“Our new Platform Trial will rapidly and cost-effectively identify which combinations of known drugs and natural products slow or stop Alzheimer’s in small groups of patients. Philanthropic support allows us to ‘de-risk’ this effort, so that the most promising products can then move on to more expansive Phase III clinical trials, in collaboration with pharmaceutical and biotech partners.”
The next step is to test their effectiveness in patients. Dr. Tanzi and his team hope to launch a Platform Trial, which allows for the testing of multiple drug combinations simultaneously — an approach used successfully in cancer research, and, most recently, in ALS — significantly reducing the time and cost to evaluate the effectiveness of these compounds on Alzheimer’s pathology.
“Our new Platform Trial will rapidly and cost-effectively identify which combinations of known drugs and natural products slow or stop Alzheimer’s in small groups of patients,” says Dr. Tanzi. “Philanthropic support allows us to ‘de-risk’ this effort, so that the most promising products can then move on to more expansive Phase III clinical trials, in collaboration with pharmaceutical and biotech partners.”
This work represents an exciting new era in the development of effective treatments for Alzheimer’s disease and related dementias, Dr. Tanzi says.
“Our new approach has the potential to end this horrific disease and change the landscape of brain health in a highly democratized manner by repurposing safe, effective and affordable combinations of known drugs to treat and prevent Alzheimer’s disease,” he says.
To learn more about Mass General Neuroscience, click here, and to learn how you can help advance promising therapies for Alzheimer’s disease, contact us.